What is the Heimlich Maneuver? How to?
What is the Heimlich Maneuver?
Choking due to a foreign object becoming lodged in the throat is a situation that can commonly occur, especially in babies and children. This blockage prevents breathing by obstructing the airway, requiring quick intervention through first aid techniques. If not dealt with immediately, the foreign object in the throat can cause asphyxiation, leading to death. In such sudden situations, there is often no time to contact health services or wait for medical help to arrive. Therefore, knowing first aid techniques is crucial, as they can save lives in these scenarios. One of the essential first aid techniques everyone should be familiar with is the Heimlich maneuver, which removes the foreign object blocking the throat and clears the airway. This can save the patient's life.
What is the Heimlich Maneuver?
The Heimlich maneuver is a first aid technique developed by Henry Heimlich in 1974 to remove foreign objects lodged in the throat. Prior to this, choking first aid involved only back blows, but it was found that the Heimlich maneuver was more effective in conscious patients. This led to a combination of back and abdominal thrusts being used in first aid. If a foreign object becomes lodged in the windpipe or throat and is not removed, it can block the airway and result in choking. This can occur in both children and adults at any time. In adults, choking often happens when a piece of food becomes stuck in the airway, while in children, it can be due to food or non-food items, such as small toys, being put into the mouth. Particularly in children under the age of three, who tend to put everything in their mouths, choking due to foreign objects is a significant risk. There is only a brief window for first aid before the lack of oxygen to the brain leads to irreversible damage. If the situation is not handled promptly, blood oxygen levels decrease, brain cells begin to die due to the lack of oxygen, and without intervention, the person will ultimately die. To be prepared for such an incident, every individual should learn about the life-saving Heimlich maneuver and be ready to perform it if necessary.
When Should the Heimlich Maneuver Be Used?
Choking can occur in adults, children, and babies if a foreign object enters the airway. The universal sign of choking, recognized by everyone, is when hands are clasped around the throat. For those unable to make this gesture or in infants and small children, important signs of choking include:
- Inability to speak, make sounds, or breathe
- Difficulty or noisy breathing
- Wheezing sounds as the person tries to breathe
- Weak or severe coughing
- Changes in skin color, lips, and under the nails turning dark or blue
- Reddening of the face, followed by a pale or bluish tint
- Loss of consciousness
If a person shows signs of choking or indicates that they are choking, the bystander should be prepared to perform the Heimlich maneuver.
How to Perform the Heimlich Maneuver
Performing the Heimlich maneuver correctly and at the right moment is critical to saving a choking victim. If the person showing signs of choking can cough strongly, they should be encouraged to continue coughing. If they are unable to speak, respond, or breathe, the "five-and-five" approach is recommended:
- If the choking person is an adult, stand behind them; if it's a child, kneel down. Place one arm across the person's chest for support and have them lean forward so that the upper body is parallel to the ground. Deliver five firm back blows between the shoulder blades using the heel of your hand. If this does not dislodge the object, proceed to the Heimlich maneuver.
- To perform the Heimlich maneuver, stand behind the person and wrap your arms around their waist. Make a fist with one hand and place it slightly above the belly button and below the rib cage. Grasp the fist with the other hand. While the person remains slightly bent forward, perform five quick upward thrusts, pressing firmly into the abdomen as if trying to lift them upward. The goal is to force air from the lungs to expel the object.
- For pregnant or obese individuals, the hands should be positioned higher, just above the point where the lower ribs meet, rather than below the rib cage.
- If you are alone, perform five back blows followed by five abdominal thrusts before calling emergency services. If a second rescuer is present, emergency services should be called immediately.
- If the object is not dislodged, continue alternating between five back blows and five abdominal thrusts until the object is removed. If the person's consciousness is lost, lay them on their back and begin basic life support. Standard CPR includes chest compressions and rescue breaths.
How to Perform the Heimlich Maneuver on Infants
If a foreign object becomes lodged in the airway of a baby under the age of one, the following first aid steps should be taken:
- Sit down and place the infant face-down on your forearm, resting your forearm on your thigh. Support the baby's head and neck with your hand, ensuring the head is lower than the chest.
- Deliver five gentle but firm back blows to the middle of the baby's back using the heel of your hand. Keep your fingers pointing upward to avoid hitting the baby's head.
- If the object is not expelled and the baby is still not breathing, turn the infant over so they are face-up on your forearm, with the head still lower than the chest. Use two fingers to apply five quick chest compressions on the breastbone.
- If breathing does not resume, call for medical help while continuing the cycle of five back blows and five chest compressions until help arrives. Be cautious not to apply excessive force to avoid damaging internal organs or ribs.
If back blows and the Heimlich maneuver fail to clear the airway and consciousness is lost, begin CPR or chest compressions for basic life support.
Choking incidents can happen to anyone, from children swallowing small objects during play to adults choking on food while eating. In many cases worldwide, lives could be saved with simple first aid techniques to dislodge objects from the airway, but a lack of first aid knowledge often leads to fatalities. To prevent this, everyone should be informed about the Heimlich maneuver and be prepared to use it to save themselves or someone else in an emergency.
By learning the Heimlich maneuver and its application techniques, you can be prepared to provide life-saving first aid during choking incidents, potentially saving lives in critical moments.
What İs Aspiration Pneumonia?
Aspiration can be defined as the accidental entry of substances intended to reach the stomach into the respiratory tract. These materials, which mistakenly enter the respiratory system during swallowing, can reach the lungs and cause serious complications. Aspiration can occur due to various reasons.
What is Aspiration?
Under normal circumstances, food, saliva, or any other material passes through the pharynx, esophagus, and stomach. On the other hand, air taken through the nose or mouth passes through the pharynx, larynx, trachea, bronchi, and into the lungs. The correct passage of both swallowed substances and air is controlled by a small structure called the epiglottis. During breathing, the epiglottis moves upward, allowing air to pass directly into the larynx. During swallowing, the epiglottis tilts downward, covering the trachea and preventing substances from entering the respiratory tract.
Aspiration occurs when the balance and coordination between swallowing and breathing controlled by the epiglottis are disrupted. In aspiration, materials that should progress to the stomach accidentally enter the trachea, which can have serious health consequences.
Aspiration primarily affects infants, the elderly, and individuals with swallowing disorders. While aspiration may occur without any noticeable symptoms, it can sometimes lead to severe symptoms, such as:
- Feeling of something stuck in the throat
- Pain or difficulty swallowing
- Coughing after eating or drinking
- Sensation of choking while eating
- Making gurgling sounds when swallowing
Additional symptoms that may develop in individuals experiencing aspiration include:
- Excessive saliva in the mouth
- Chest discomfort
- Heartburn
- Fatigue or shortness of breath while eating
- Fever developing shortly after meals (within about 30 minutes)
- Difficulty chewing
- Frequent pneumonia episodes
Aspiration is also common in infants. Some aspiration symptoms in infants are:
- Poor sucking reflex
- Facial redness or grimacing during feeding, with watery eyes
- Rapid or interrupted breathing while feeding
- Mild fever after feeding
- Wheezing and other respiratory problems
- Frequent respiratory infections or pneumonia
What Causes Aspiration?
Aspiration can develop for different reasons in adults and infants.
Causes of Aspiration in Adults
The primary cause of aspiration in adults is impaired swallowing function. When swallowing does not occur normally, the mechanisms preventing aspiration may fail, leading to substances entering the respiratory tract. The main causes of aspiration in adults include:
- Loss of Tongue Control: The tongue is a muscular organ controlled by nerves. Loss or weakening of this control can impair the swallowing reflex, leading to aspiration, especially of liquids.
- Abnormal Swallowing Reflex: A dysfunctional swallowing reflex allows food or other materials to enter the airway.
- Neurological Diseases: Conditions like Parkinson’s disease can impair tongue control and cause aspiration.
- Esophageal Disorders: Problems with the esophagus, such as gastroesophageal reflux disease (GERD), dysphagia (painful swallowing), or throat cancer, can contribute to aspiration.
- Neck Surgery: Surgical procedures affecting the larynx can disrupt swallowing. If the epiglottis is damaged, the coordination between breathing and swallowing may be compromised.
- Oral and Dental Problems: Dental issues can impair chewing and swallowing, increasing the risk of aspiration.
- General Anesthesia: During surgeries, the contents of the stomach may flow back into the respiratory tract, posing a risk of aspiration. Surgical teams take precautions to prevent this by requiring patients to fast before procedures.
Causes of Aspiration in Infants
In infants, aspiration often occurs due to swallowing dysfunction related to issues with the throat muscles. Conditions that may weaken the throat muscles in infants include:
- Physical abnormalities like cleft palate
- Growth retardation
- Brain damage
- Nerve damage
- Neuromuscular disorders such as cerebral palsy or spinal muscular atrophy
What Are the Complications of Aspiration?
Aspirating solid or liquid substances can lead to serious health problems.
Aspiration Complications in Adults
Aspiration can result in severe issues, including infections and tissue damage. One of the most serious complications is aspiration pneumonia, which occurs when materials entering the lungs cause an infection. Aspiration pneumonia leads to inflammation and fluid accumulation in the lungs. Its symptoms may develop slowly over time and include:
- Frequent coughing with foul-smelling sputum
- Shortness of breath
- Fever, sweating, and chills
- Chest pain or the need to cough when taking deep breaths
- Anxiety, fatigue, or confusion
- Feeling of suffocation
Aspiration Complications in Infants
In infants, aspiration can lead to similar complications, including pneumonia. Additionally, chronic aspiration may result in dehydration, malnutrition, and weight loss.
How is Aspiration Diagnosed and Treated?
Early diagnosis and treatment of aspiration are crucial to prevent complications.
Diagnosis
If aspiration causes noticeable symptoms, it becomes easier to detect and diagnose. However, in some cases, symptoms may not be obvious, making diagnosis more challenging. The diagnostic process usually involves a patient interview and physical examination. The following methods may be used to diagnose aspiration:
- X-rays: These help assess the effectiveness of breathing.
- Bronchoscopy: A thin tube with a camera is inserted into the respiratory tract to view the inside of the lungs.
- Modified Barium Swallow Test: The patient swallows liquids or solids containing barium, and a series of images are taken to check for leaks into the airway.
- Fiberoptic Endoscopic Evaluation of Swallowing (FEES): A thin tube with a camera is inserted through the nose to view the throat and larynx while the patient swallows saliva or food. This helps detect any leakage into the airway.
Treatment
The primary aim of aspiration treatment is to address the underlying cause. Without resolving the root issue, eliminating aspiration completely may not be possible.
Some measures to prevent aspiration include:
- Eating small bites of food
- Remaining calm and relaxed while eating
- Softening dry foods with sauces or liquids
- Avoiding taking new bites before swallowing the previous one
- Refraining from talking while eating or drinking
- Avoiding eating or drinking while lying down
- Maintaining good oral and dental hygiene
- Avoiding smoking
Aspiration can lead to serious health problems in both adults and infants. To prevent these issues, necessary precautions should be taken during feeding. Individuals experiencing symptoms of aspiration should seek medical attention promptly. Stay healthy!
What is intubation? How is Intubation Done?
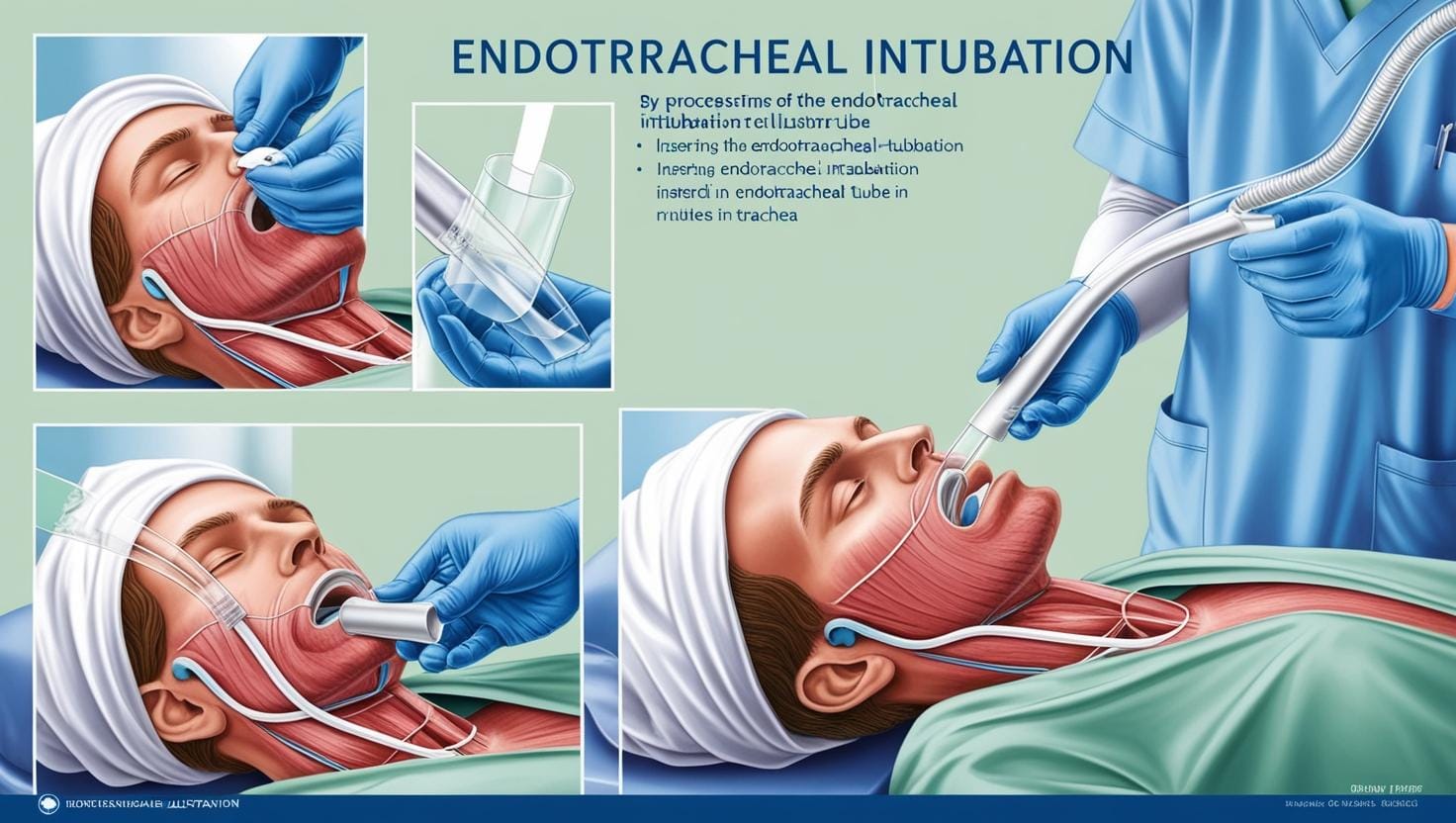
Intubation involves the insertion of a thin tube, called an endotracheal tube, through the mouth into the airway. This procedure connects the patient to a ventilator, a device that assists or takes over the process of breathing. Intubation is performed in situations where the patient requires anesthesia, sedation, or respiratory support due to a severe medical condition. It is a common medical practice today for maintaining adequate oxygen supply and airway control.
What Does "Being Intubated" Mean?
The term “intubated patient” has become widely recognized, prompting questions such as, “What does intubation mean, and why are patients intubated?” An intubated patient refers to someone who has undergone the intubation process to receive respiratory support. This is usually necessary for individuals who cannot manage their airways or breathe unassisted.
Why is Intubation Necessary?
Patients may require intubation during surgeries, especially under general anesthesia, since the drugs used affect all muscles, including the diaphragm, making independent breathing impossible. In most cases, the endotracheal tube is removed after surgery when the anesthesia wears off, allowing the patient to resume normal breathing.
However, in cases involving major surgeries like open-heart procedures or serious respiratory conditions, the tube may remain in place longer, with the patient breathing through a ventilator.
Intubation is also required in cases of respiratory failure caused by conditions such as:
- Severe lung injury
- Pneumonia
- COVID-19
How is Intubation Performed?
Before the procedure, the patient is typically under anesthesia or sedation, or unconscious due to illness, which facilitates easier access to the airway. The patient is laid flat on their back, and the clinician, positioned at the patient’s head, gently opens the mouth and advances a tube using a tool equipped with light. Pressure is applied to the tongue to prevent airway obstruction, and the tube is carefully inserted into the airway. To confirm proper placement, the clinician listens to the patient’s lungs using a stethoscope.
In some cases, nasal intubation (using a nasotracheal tube) may be performed, especially when oral access is restricted. Pediatric intubation follows the same principles but requires smaller instruments due to children’s narrower airways.
Extubation and Recovery
Once the patient no longer needs intubation, the tube is removed through a process called extubation. The balloon securing the tube is deflated, and the tube is gently withdrawn. The patient is then closely monitored for any respiratory distress, which may necessitate additional oxygen support.
Risks of Intubation
While intubation is often necessary to save lives, it carries some risks, especially if the procedure is prolonged:
- Injuries to the teeth, tongue, throat, or larynx
- Insertion of the tube into the esophagus instead of the trachea
- Tracheal injury
- Bleeding or aspiration (inhalation of fluids or food into the lungs)
- Pneumonia or lung infections
Nutrition During Intubation
For short procedures, no special feeding is required, but for extended intubation, nutrition is provided via intravenous (IV) fluids or a feeding tube. Feeding can be done using orogastric (through the mouth) or nasogastric (through the nose) tubes. These methods ensure that the patient receives necessary nutrients while intubated.
Intubation, despite its risks, is a critical medical procedure, often used to address respiratory issues caused by diseases like pneumonia, COVID-19, or chronic obstructive pulmonary disease (COPD). It ensures that patients in respiratory distress receive adequate oxygen and airway management, essential for survival in severe cases.
What are Intestinal Diseases?
Definition of Inflammatory Bowel Disease: Inflammatory bowel diseases are a term used for diseases that result from chronic inflammation in the digestive system, primarily affecting the intestines. The two most common types of inflammatory bowel diseases are ulcerative colitis and Crohn's disease.
Ulcerative Colitis: This condition primarily affects the colon and rectum. In ulcerative colitis, the superficial layer that lines the colon is affected, leading to the formation of ulcers on the intestinal surface.
Crohn's Disease: Crohn's disease can affect any part of the digestive system, but it most frequently involves the small intestine. While only the surface layer of the intestine is affected in ulcerative colitis, deeper tissues can be affected in Crohn's disease.
The symptoms of inflammatory bowel diseases vary depending on the area affected and the severity of the inflammation. Some patients may exhibit milder symptoms, while others may experience severe indications. Inflammatory bowel diseases can manifest with flare-ups when symptoms intensify and remission periods when symptoms subside. Common symptoms in ulcerative colitis and Crohn's disease include:
- Diarrhea
- Abdominal pain
- Blood in stool
- Abdominal cramps
- Loss of appetite
- Fatigue and weakness
- Unintentional weight loss
Individuals showing one or more of these symptoms or noticing changes in their bowel movements recently should consult a doctor for necessary examinations. As inflammatory bowel diseases can lead to serious health issues, their diagnosis and treatment should not be overlooked.
What are the Complications of Inflammatory Bowel Diseases?
Inflammatory bowel diseases can lead to some undesirable effects in the body. Common complications that can occur in both ulcerative colitis and Crohn's disease include:
- Colon Cancer: Patients whose large intestine has been significantly affected by ulcerative colitis or Crohn's disease have an increased risk of developing colon cancer. Patients diagnosed with inflammatory bowel cancer begin screening for colon cancer 8-10 years after diagnosis. The timing of the screening may vary based on the patient's age, comorbidities, and family history, so diagnosed patients should discuss when to start screening with their doctor.
- Skin, Eye, and Joint Inflammations: During flare-ups of inflammatory bowel diseases, conditions like arthritis (joint inflammation), skin lesions, and uveitis may occur.
- Medication Side Effects: Some medications used to treat inflammatory bowel diseases may carry a slight risk of cancer development. Corticosteroids used in treatment can also lead to conditions such as osteoporosis and high blood pressure.
- Primary Sclerosing Cholangitis: This condition, which involves the inflammation and narrowing of the bile ducts within the liver, can lead to impaired liver function. People with primary sclerosing cholangitis are likely to have inflammatory bowel disease.
- Blood Clots: Inflammatory bowel diseases increase the risk of blood clot formation within blood vessels.
Undesirable Conditions Associated with Crohn's Disease:
- Intestinal Obstruction: Crohn's disease can affect all layers of the intestinal wall, causing the affected segment to thicken and narrow, obstructing the passage of digestive materials through the intestine.
- Malnutrition: Patients with Crohn's may struggle to eat due to diarrhea, abdominal pain, and cramps. Additionally, absorption issues may occur in the intestine, leading to insufficient intake of essential nutrients. This can result in vitamin B12 and iron deficiency anemia.
- Fistula Formation: A fistula refers to an abnormal connection between two different parts of the body. In Crohn's disease, inflammation of the intestinal wall can lead to the formation of fistulas connecting to other organ walls, most commonly occurring in the anal region. A fistula may become infected and form an abscess.
- Anal Fissure: Patients with Crohn's may develop small tears in the skin around the anus, known as anal fissures.
Complications Seen in Ulcerative Colitis:
- Toxic Megacolon: In patients with ulcerative colitis, the colon may suddenly swell and expand, leading to a condition called toxic megacolon.
- Intestinal Perforation: Toxic megacolon can cause intestinal perforation, which can occur spontaneously.
- Severe Fluid Loss: Excessive fluid loss due to diarrhea can lead to dehydration.
What Causes Inflammatory Bowel Diseases?
The exact causes of inflammatory bowel diseases remain unclear. Experts believe that various factors, including diet, genetics, stress, and environmental factors, may play a role in disease development.
The immune system also plays a role in the development of inflammatory bowel diseases. Under normal circumstances, the immune system recognizes and destroys harmful microorganisms such as bacteria, viruses, and parasites that enter the digestive system. During this process, inflammation occurs in the intestine to combat the infection. Once the infection is resolved, the inflammation subsides, and the intestine returns to its normal state. In healthy individuals, the infection process operates in this manner. However, in inflammatory bowel diseases, inflammation occurs in the absence of an infection. The immune system attacks the healthy intestinal cells, leading to organ damage.
Risk Factors for Inflammatory Bowel Diseases:
- Age: Patients diagnosed with inflammatory bowel diseases are often under 30, though some may not develop the disease until their 50s.
- Family History: Individuals with first-degree relatives (parents, siblings, children) who have inflammatory bowel diseases are at a higher risk.
- Smoking: Smoking is the most significant controllable risk factor for developing Crohn's disease.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Medications containing active ingredients like ibuprofen, naproxen sodium, and diclofenac sodium pose risks for both the development of the disease and the progression of existing conditions.
Diagnosis and Treatment of Inflammatory Bowel Diseases:
Diagnosis involves a comprehensive investigation considering other disorders that could cause similar symptoms and signs. Blood tests and stool tests are performed to evaluate potential diseases. Endoscopy and colonoscopy are used to assess the effects of ulcerative colitis or Crohn's disease on the digestive organs. For patients with conditions like intestinal perforation where endoscopic methods cannot be applied, imaging methods such as X-ray, CT, or MRI may be utilized.
The primary goal in treating inflammatory bowel diseases is to reduce the inflammation causing the disorder. Reducing inflammation alleviates both symptoms and signs, contributing to long-term remission of the disease. Additionally, treatment can help prevent complications that may arise from the disease.
Both medication and surgical methods can be employed in treatment.
In Medication Treatment:
- Anti-inflammatory medications such as corticosteroids to reduce inflammation.
- Immunosuppressive drugs like azathioprine and methotrexate to suppress the immune response.
- Antibiotics may be used if an infection develops due to the disease.
- Depending on the patient's condition, the doctor may prescribe anti-diarrheal, pain relief medications, and vitamin supplements.
When significant weight loss occurs or nutritional intake severely declines in patients with inflammatory bowel disease, nutritional support may be initiated. Specialized nutritional methods, such as tube (enteral nutrition) or intravenous nutrition (parenteral nutrition), may be implemented to facilitate recovery and rest the intestine.
In the surgical treatment of ulcerative colitis and Crohn's disease, the affected section of the intestine is removed, allowing the remaining intestine to function healthily. Surgical intervention may also be necessary for complications such as intestinal obstruction. However, surgery does not provide a definitive solution for these diseases. The operation is performed to improve the patient's overall condition and prevent possible complications.
If you suspect you have inflammatory bowel disease, consult a qualified healthcare facility for necessary examinations. It is beneficial for individuals diagnosed with inflammatory bowel disease to consult a gastroenterologist to discuss the most effective treatment methods and obtain detailed information about the disease.
Wishing you healthy days.
What is a Steam Machine, and How is it Used in Healthcare?
Low humidity levels (below 30%) can lead to various issues, such as dry skin, nosebleeds, and respiratory problems. During cold and flu season, dry air can further worsen breathing issues.
To combat the negative effects of dry air, humidifiers are a practical solution. Devices like steam vaporizers and cool mist humidifiers add moisture to the air, providing relief from congestion and cold symptoms. Each humidifier type offers different ways of releasing moisture into the environment. You can buy these humidifiers from pharmacies, stores, or online platforms.
What is a Steam Vaporizer?
A steam vaporizer aims to alleviate dryness that could irritate the body, especially in the nose, throat, lips, or skin. It can also help ease symptoms caused by colds or the flu. However, excessive use may aggravate respiratory issues, so it’s important to use these devices correctly.
When Should You Use a Humidifier?
Humidifiers prevent dryness, acting as a natural remedy for:
- Dry skin
- Sinus congestion and headaches
- Irritated throat
- Bloody nose
- Dry cough
- Cracked lips
- Vocal cord irritation
Types of Humidifying Machines
- Steam Vaporizer: Electric-powered and portable, ideal for short-term use. However, these pose a burn risk, especially for children.
- Ultrasonic Cool Mist Humidifier: Uses ultrasonic vibrations to generate cool mist, available in models that offer both cool and warm mist. It’s safer for children since it doesn’t involve boiling water.
- Additional Types:
- Central humidifiers
- Evaporators
- Impeller humidifiers
- Ultrasonic humidifiers
Size and Portability of Humidifiers
Humidifiers come in two main categories:
- Console units: Suitable for larger spaces or entire homes.
- Portable units: Small and easy to carry, ideal for travelers.
Monitoring Humidity Levels
While adding moisture can relieve dryness, excessive humidity may cause mold, dust mites, and respiratory issues. According to Mayo Clinic, maintaining a humidity level between 30-50% is recommended. A hygrometer can help monitor indoor humidity levels, especially in households with allergies or asthma.
Risks of Using a Humidifier
- Burns: Steam vaporizers pose a burn risk, especially for children.
- Mold and Dust Mites: Excess moisture can encourage the growth of harmful allergens.
- Bacterial Growth: Dirty humidifiers can spread bacteria, aggravating respiratory issues. Regular cleaning and maintenance are crucial.
- Mineral Release: Use distilled water to minimize the release of minerals into the air.
Experts generally recommend cool mist humidifiers to avoid burn risks associated with hot steam. Both types of humidifiers improve respiratory health but achieve this through different mechanisms.
How is the Use of Humidifiers in Babies and Children?
According to the Centers for Disease Control and Prevention (CDC), human parainfluenza viruses are a common cause of respiratory infections in children, such as croup and bronchiolitis. Both illnesses can cause nasal congestion and coughing, reducing moisture. Therefore, adding humidity to the air helps relieve a stuffy nose and is especially beneficial for babies and young children who cannot blow their noses.
When choosing between warm or cool mist humidifiers, it's essential to consider what is suitable for specific age groups. For example, warm mist is not a good option for use around children, as it can cause burns if knocked over due to boiling water. A cool mist humidifier, which does not pose a burn risk, is a better choice for children.
In conclusion, both cool and warm mist humidifiers add moisture to the air and can help relieve respiratory discomfort without medication. Both devices also help alleviate skin and nasal dryness. Ultimately, the type of machine you choose depends on your personal health, budget, age, and other factors related to your family’s health.
Regardless of the situation, using a humidifier requires caution, and you should not use it if your health does not warrant it. First, ensure that you monitor the humidity levels in the environment to prevent indoor allergies. Consult an allergist before deciding to use one. To ensure safe operation, clean your machine daily while in use, and strictly follow the operating instructions. If you have respiratory issues such as asthma or bronchitis, consult your doctor before deciding to use a humidifier.