🩺 What Are the Symptoms of Drug Allergy? How to Relieve Itching?
In daily life, some people may develop a drug allergy when using certain medications. This reaction is an unexpected response from the immune system to the drug. If you experience such a reaction, the diagnosis of a drug allergy should be made accurately by a healthcare professional. Drug side effects and drug allergies are different and should not be confused. Drug allergies can also develop in children, but adults have a higher risk of developing drug allergies.
What is a Drug Allergy?
A drug allergy is an unexpected immune response that occurs shortly after using a drug at the correct dose and through the right administration method. These reactions can manifest as minor symptoms like rashes and itching, but they can also lead to severe cases like anaphylactic shock. Anaphylaxis can be life-threatening.
What Are the Symptoms of a Drug Allergy?

Drug allergy symptoms can vary from person to person. The most common symptoms include:
- Rash and redness on the skin
- Urticaria (Hives)
- Fever
- Itching
- Runny nose
- Swelling of the face and body
- Difficulty breathing
- Wheezing
- Anaphylaxis
- Abnormal liver and kidney values
Drug allergy symptoms may appear within a few hours after taking the medication or even days later. The symptoms may initially seem insignificant but may gradually worsen. Skin rashes that appear harmless initially can lead to shortness of breath and progress if drug usage continues.
Drug allergy and drug side effects are two issues that should not be confused. Drug allergies are unexpected immune reactions, whereas drug side effects are known possible reactions that can be anticipated and even categorized into risk groups.
What Are the Causes of Drug Allergy?
It is not possible to specify exact causes for drug allergies. Since everyone’s immune system functions uniquely, the causes of drug allergies vary from person to person. While drug allergies are not very common, the frequency of allergic reactions has increased in recent years with the development of new medications. Certain situations may act as risk factors for drug allergies.
These situations include:
- A history of known allergies, such as taking spring allergy medications
- A history of multiple drug use
- A family history of drug allergy
- Genetic factors
- Certain viral infections (e.g., HIV, EBV)
- Age
The incidence of drug allergies is higher in young and middle-aged adults. Additionally, drug allergies are more common in women than in men. Oral (by mouth) drug use has a lower allergy risk, whereas administering the drug intramuscularly or intravenously increases the risk.
This is due to the rapid and high-dose absorption of the drug into the body via these routes. It is recommended to wait 15-30 minutes at a healthcare facility after intramuscular or intravenous injections. Most allergic reactions occur within the first 15 minutes following infusion.
How is Drug Allergy Diagnosed?
Several methods can diagnose a drug allergy. First, a patient history is taken, followed by a thorough physical examination, and then tests may be ordered based on the medications used. Skin allergy testing and blood tests may be requested for diagnosis.
In skin allergy testing, specific allergenic substances are applied to tiny incisions on the skin. The allergen is determined by observing which spot shows swelling. In blood tests, specific immunoglobulin E (IgE) is usually checked in the serum. For more detailed research, the suspected drug may be administered under controlled conditions to diagnose which drug caused the allergy and how the reaction developed.
How is Drug Allergy Treated?
First, the use of the drug that caused the allergy is discontinued under the supervision of a doctor. A doctor may prescribe another drug with the same function but a different active ingredient.
If the medication cannot be discontinued, a procedure known as “desensitization” can be administered under the supervision of an allergy specialist in a hospital. In the desensitization method, the drug is gradually introduced into the body at very low doses, allowing the body to adjust to the medication.
Minor symptoms caused by drug allergies, such as rashes and redness, can be treated with corticosteroid or antihistamine medications. For this, it is recommended to consult an allergy and immunology specialist. For cases of drug allergies in children, consulting a pediatric immunologist is advisable.
The most severe symptom is anaphylactic shock, and in the event of anaphylaxis, it is crucial to seek emergency medical care. In the case of shock, swelling in the airways may prevent breathing, and the person may even lose consciousness.
In such cases, intubation may be required. Swelling in the airways is caused by angioedema, where fluid from blood vessels passes into the tissues, resulting in swelling known as edema. Swelling is most common in the head, neck, and extremities.
Frequently Asked Questions About Drug Allergy
Do Spring Allergy Medications Cause Allergies?
Many people with pollen allergies use medications, but as with any drug, spring allergy medications can also trigger allergic reactions. Though rare, all symptoms from simple skin rashes to systemic reactions may occur. Therefore, allergies to allergy medications themselves can develop. In addition, pollen allergy medications may cause side effects such as drowsiness, numbness, dry mouth, and dizziness.
How to Relieve Itching from Drug Allergy?
Itching from drug allergies can be relieved with topical creams or oral antihistamine tablets prescribed by a doctor. Antihistamines help prevent the immune system from developing an allergic reaction.
Applying cold compresses to the itchy area can also help reduce blood flow and alleviate itching. In addition, taking a warm shower, wearing loose-fitting clothes, and applying moisturizing lotions can help reduce itching. It is best to avoid excessive scratching in the affected area.
How Long Does a Drug Allergy Last?
Drug allergies may develop within the first hour after taking the drug, known as an early reaction. Reactions occurring after an hour are called delayed reactions. The duration of the allergy depends on the severity of the symptoms and the individual’s immune system, and it can vary. Allergic reactions should be treated as soon as they are noticed.
What Herbal Remedies Help with Drug Allergies?
Drug allergies result from the chemical components in medications and should be treated with the drugs recommended by a doctor. Therefore, herbal products should not be used to treat drug allergies without a doctor’s recommendation. Herbal remedies may accelerate the effect of the drug that triggered the allergy and may worsen the reaction, leading to severe consequences like shortness of breath and loss of consciousness.
What Helps with Lip Swelling from Drug Allergy?
Antihistamine medications and cold compresses can help relieve lip swelling due to a drug allergy. Anti-inflammatory medications recommended by a doctor can help reduce swelling and alleviate pain, if any. However, it is essential to discontinue the use of the drug causing the swelling in the first place.
How is Drug Allergy Diagnosed?
There is no way to detect a drug allergy in advance. However, after using a drug, symptoms that appear can lead to a diagnosis through a detailed patient history, blood tests, and allergy tests conducted by a healthcare provider.
By combining all findings, a diagnosis can be made. If redness, rash, itching, and swelling occur shortly after drug intake, especially around the face, eyes, and mouth, and if there is difficulty breathing, this may indicate a drug allergy.
🦠 COVID Symptoms 2024
COVID-19 Symptoms and What to Do
Understanding the symptoms of COVID-19 2024 is crucial for early detection and management. Below is a comprehensive table outlining common symptoms of COVID-19, along with guidance on what actions to take if you or your child exhibits these symptoms.

Symptoms of COVID-19
| Symptom | Description |
|---|---|
| High Temperature | A high temperature indicates you feel hot to touch, especially on the chest or back (no need to measure). |
| New, Continuous Cough | Coughing frequently for more than an hour or having three or more coughing episodes within 24 hours. |
| Loss or Change in Taste/Smell | A noticeable loss or alteration in your sense of taste or smell. |
| Shortness of Breath | Difficulty breathing or feeling breathless. |
| Fatigue | Unusual tiredness or exhaustion that doesn’t improve with rest. |
| Aching Body | General body aches and discomfort. |
| Headache | Persistent pain in the head. |
| Sore Throat | Pain or irritation in the throat. |
| Blocked or Runny Nose | Nasal congestion or excessive mucus. |
| Loss of Appetite | Decreased desire to eat or drink. |
| Diarrhoea | Frequent, loose, or watery stools. |
| Nausea or Vomiting | Feeling sick or actually vomiting. |
What to Do If You Have Symptoms
If you or your child exhibits symptoms of COVID-19, consider the following steps:
- Stay Home: Isolate at home and avoid contact with others, especially if experiencing a high temperature or feeling unwell.
- Monitor Symptoms: Return to normal activities only when feeling better and no longer have a high temperature.
- For Mild Symptoms in Children: If your child has mild symptoms (e.g., runny nose, sore throat), they may attend school or childcare if they feel well enough.
Self-Care for COVID-19 Symptoms
While treatment options may vary, you can take measures to ease symptoms:
Do's
- Rest: Ensure plenty of rest to aid recovery.
- Stay Hydrated: Drink plenty of fluids; urine should be light yellow or clear.
- Pain Relief: Use paracetamol or ibuprofen for discomfort.
- Honey for Cough: A teaspoon of honey may help with a cough (avoid giving honey to babies under 12 months).
- Manage Breathlessness: Open windows for airflow, sit upright, and lean slightly forward to ease breathing.
Don’ts
- Avoid Lying Flat: If coughing, lie on your side or sit up to breathe easier.
- No Fans: Do not use fans as they may spread the virus.
- Stay Calm: Try not to panic if experiencing breathlessness, as it may worsen symptoms.
What to Do If You Test Positive
If you or your child tests positive for COVID-19, follow these guidelines:
- Isolate: Stay home for:
- 3 days for children under 18.
- 5 days for adults 18 and over.
- Limit Contact: Avoid close contact with vulnerable individuals for 10 days.
- Testing: No longer required to take a COVID-19 test if symptomatic.
When to Seek Urgent Medical Help
Contact healthcare services if you notice:
- Symptoms worsening or not improving.
- Signs of other illnesses (e.g., rash, loss of appetite).
- High temperature lasting more than 5 days.
Urgent Actions: Call 999 or visit A&E if experiencing:
- Sudden chest pain or severe breathlessness.
- Coughing up blood.
- Unusual symptoms in children (e.g., not responding, rash that doesn’t fade).
Conclusion
Recognizing COVID-19 symptoms and knowing how to respond is vital for health and safety. If you have concerns or need assistance, do not hesitate to contact a healthcare professional. Stay informed and take proactive measures to protect yourself and others from the virus.
💊🍊✨💪 What Is A Methylated Multivitamin?
Methylated Multivitamins: Understanding Their Importance and Benefits
Methylation is a vital process that your body uses to turn genes on and off. Unfortunately, approximately 30-40% of the population carries genetic mutations that hinder efficient methylation. Even in individuals without these genetic predispositions, factors such as age, gender, lifestyle, and diet can interfere with the body’s ability to produce and utilize essential methyl groups. Methylated multivitamins can help bridge this gap, but are they the right choice for everyone? Let's explore.
What is Methylation?
Methylation is an essential biochemical process that regulates gene expression, cellular function, and the activity of critical organ systems, including the cardiovascular, reproductive, and central nervous systems. It also influences other vital molecules, such as proteins, lipids, and hormones.
Key functions affected by methylation include:
- Energy Production
- Neurotransmitter Regulation
- Hormonal Balance
- Histamine Management
- Liver Function
- DNA Replication and Growth Processes
The Role of DNA in Methylation
DNA is the blueprint of life, containing genes that determine our physical characteristics and regulate our body’s functions. The average human has between 20,000 and 25,000 genes, but only a fraction is active at any given time. Methylation plays a crucial role in gene regulation, essentially determining which genes are expressed and which are silenced. This process ensures that cells can specialize; for example, a skin cell behaves like a skin cell and not a brain cell.
Consequences of Poor Methylation
Various factors can disrupt methylation, leading to what is termed poor methylation. Common disruptors include:
- Stress
- Age
- Environmental Toxins
- Gut Health
- Poor Nutrition
Poor methylation can lead to several health issues, including chronic fatigue, hormonal imbalances, cognitive impairment, and conditions like Alzheimer’s and Parkinson’s. Signs of poor methylation may include:
- Depression
- Anxiety
- Fatigue
- Memory Issues
- Brain Fog
- Chronic Inflammation
- Insomnia
- Headaches
What are Methylated Multivitamins?
For individuals facing methylation challenges, methylated multivitamins can be particularly beneficial. These supplements contain active methyl groups, making them easier to absorb and utilize. Methylated multivitamins can enhance mood, cognitive function, boost energy levels, and improve sleep quality.
Common methylated vitamins include various B vitamins, particularly:
- Methylcobalamin (B12)
- 5-Methyltetrahydrofolate (5-MTHF) (B9)
- Pyridoxal-5-Phosphate (B6)
By supplementing with these forms, individuals can obtain methyl groups without depleting their stores.
Are Methylated Multivitamins Superior?
In general, methylated multivitamins offer enhanced absorption and bioavailability. However, they are not suitable for everyone. Some individuals may experience overmethylation, a condition characterized by excessive methyl group production, leading to potential side effects such as:
- Rapid Speech
- Hyperactivity
- Dry Eyes and Mouth
- Paranoia
- High Pain Threshold
- Sleep Disorders
Overmethylation is often linked to excessive copper intake, either through supplements or a diet rich in copper-containing foods, such as oysters and organ meats. For those experiencing overmethylation, it's advisable to avoid methylated multivitamins.
Foods to Enhance Methylation
For those looking to boost their methylation without relying solely on supplements, several foods can help:
- Dark Leafy Greens: Spinach, collards, and turnip greens are high in methyl-rich folate (B6).
- Beets: Known for their high betaine content, beets provide naturally occurring methyl groups and may improve cognitive function.
- Turmeric: Rich in choline, turmeric is a powerful methylation adaptogen. Using fermented turmeric can enhance both its benefits and flavor.
- Liver and Organ Meats: These foods are excellent sources of copper and folate, which support methylation.
- Mushrooms: Particularly shiitake mushrooms are rich in choline, copper, selenium, and B vitamins, promoting better methylation.
Methylated multivitamins can play a crucial role in supporting methylation, especially for individuals with genetic predispositions or other factors that disrupt this essential process. By choosing the right supplements and incorporating methylation-friendly foods into your diet, you can help improve your overall health and well-being. However, always consult a healthcare professional before starting any new supplement regimen to ensure it's suitable for your individual needs.
What are the harms of Botox?
Harms of botox include a range of potential side effects that should be carefully considered. Common concerns associated with botox treatments are allergic reactions, visual deformities due to improper application, and rapid loss of effect. Alongside these potential drawbacks, understanding the side effects of botox is essential for anyone contemplating this treatment.
To mitigate these adverse effects, it is crucial to undergo botox under the supervision of a certified professional and to follow their guidance closely. For many years, botox has been utilized in both medical and aesthetic applications, emphasizing the need to balance benefits with risks.
What is Botox?
Botox is a neurotoxic protein containing botulinum toxin type A and bacteria from the Clostridium botulinum family. When injected, it temporarily immobilizes the muscles in the treated area, significantly reducing wrinkles and other functional issues.
Used for both medical and cosmetic purposes, botox’s effects typically last 3 to 8 months, depending on the area of application. While its history dates back to 1817, it was first used in humans in 1973, receiving medical approval in 1989.
In the early second quarter of 2002, botox received FDA approval for reducing frown lines and underarm sweating. Today, it is widely popular, with 90% of users being women and 10% men.

What Are the Side Effects of Botox?
Though botox can be used for medical purposes, it is most commonly chosen for cosmetic enhancements. Facial botox is among the most popular treatments, especially for wrinkles on the forehead, between the brows, and around the mouth. Both men and women seek botox to temporarily smooth lines and wrinkles on the face.
As with any procedure, there is a chance of side effects. The potential risks of botox include:
- Gradual loss of effect
- Overexposure to toxins due to excessive injections
- Infection risk at the injection site
- Potential for permanent damage in the treated area
- Visual deformities resulting from improper application
- Allergic reactions in the treated area
- Side effects for pregnant and breastfeeding women
- Temporary side effects like headaches, eyelid drooping, and dry eyes
Some of these side effects may be short-lived, while others could impact quality of life with longer-lasting or even permanent consequences. Therefore, it is essential that botox be administered by certified experts to minimize risks.
Side Effects of Botox for Men
Collagen loss due to aging affects men just as much as women. Men who wish to prevent wrinkles and fine lines caused by loss of facial elasticity also opt for botox. The side effects of botox can manifest as unwanted reactions in men, similar to women.
However, given the differences between male and female anatomy, the effects of botox can vary between the genders. Men often choose botox for the scalp, between the brows, and around the eyes. This treatment in men is sometimes referred to as "brotox."
In addition to facial botox, botox is also used in men for conditions such as bladder dysfunction, benign prostatic hyperplasia, painful bladder syndrome, and premature ejaculation. While botox continues to be studied in urology, it is known to be applied to patients who do not respond to other treatments.
For example, the success rate of bladder botox is reported to be between 75% and 80%, with an average effect duration of 1 to 3 years. Patients should be informed about the temporary nature of this treatment to avoid any disappointment when the effects wear off.
Side Effects of Botox for Women
Botox should only be administered by qualified professionals. Although it has been globally approved, when done by unlicensed individuals, it can become dangerous. Those considering botox are strongly advised to seek out certified experts. The dose used in botox is crucial; the lower the dose, the fewer the side effects.
Botox is frequently chosen not only for cosmetic reasons but also for teeth grinding, chronic migraines, and excessive sweating. During pregnancy and breastfeeding, however, botox is generally discouraged.
Even though data is limited, it is assumed that botulinum toxin could potentially cross the placenta and harm the fetus. Similarly, botox is not recommended during breastfeeding.
Anyone considering botox during pregnancy or breastfeeding should consult a professional to discuss the appropriate timing and dose. Expert advice is essential for understanding the side effects and potential risks.
Side Effects of Botox
The benefits and side effects of botox are subjects of frequent discussion. When botox is applied correctly, its side effects are generally minimal. However, the most common side effects of botox include:
- Food poisoning
- Eyelid drooping
- Headache
- Swelling and bruising at the injection site
- Eyebrow twitching
- Numbness around the treated area
- Temporary paralysis of nearby muscles
- Pain, redness, or edema at the injection site
- Mild nausea
- Fever, chills, dry mouth
- Double vision or reduced vision
- Bleeding and swelling
These side effects, which occur in only 1–2% of patients, are generally rare and temporary. When botox is administered by trained professionals, the side effects are typically minimal, making it a safe option.
Since botox provides desired results without surgery, it offers an additional advantage. However, it is essential for patients and doctors to discuss and agree on both the benefits and risks before the treatment.
Frequently Asked Questions About Botox
How Many Types of Botox Are There?
Botox can be applied to various areas, including the chin, lips, brows, forehead, between the brows, around the eyes, cheeks, for sweating, bladder issues, and migraines.
What is the Difference Between Botox and Fillers?
Botox and fillers are often confused but are two different treatments. Botox uses a toxin, whereas fillers use hyaluronic acid, a protein found naturally in the human body.
Fillers are mainly used to correct shape irregularities in the treated area, while botox blocks muscle activity to keep the area firm. Their effects also differ in duration.
What Precautions Should Be Taken After Botox?
After a botox application, the treated area should not come into contact with water for at least 6 hours. Additionally, it is recommended to avoid physical exercise, bending forward, and sleeping face down for the duration specified by the doctor.
Avoiding hammam, sauna, and alcohol is also important to maintain the effect of botox.
Is Botox a Safe Procedure?
Botox is an FDA-approved procedure, also approved by our Ministry of Health. It has shown success in treating various conditions, including strabismus, throat pain during swallowing, and muscle relaxation, though it is primarily recognized for its effectiveness in aesthetic applications.
What is Gum Botox and Jaw Botox (Masseter Botox)?
Gum botox and jaw botox (masseter botox) have become popular in recent years for both aesthetic and functional purposes. These types of botox are used to enhance gum appearance and relax jaw muscles.
What is Gum Botox?
Gum botox is a cosmetic procedure designed to prevent excessive gum exposure during smiling. Some individuals find that too much of their gum tissue shows when they smile, a concern known as a gummy smile. To address this, botulinum toxin (botox) is injected into the upper lip muscles, reducing the visibility of the gums and creating a more balanced smile.
This procedure is minimally invasive, with quick recovery and a short treatment time. Performed under local anesthesia, gum botox typically lasts 3–4 months and can be repeated as needed. When administered correctly, it provides a natural, pleasant smile, making it a safe and effective option.
What is Jaw Botox (Masseter Botox)?
Jaw botox, also known as masseter botox, is a cosmetic and functional procedure in which botulinum toxin is injected into the masseter muscles.
These muscles are primarily responsible for chewing, and in some cases, they may become overactive, resulting in a wider jawline, square facial structure, or teeth grinding (bruxism). Jaw botox helps by reducing the activity of these muscles, creating a slimmer jawline and a more oval face shape.
It is also an effective treatment for teeth grinding and jaw tension. Overactive masseter muscles can lead to jaw pain, headaches, and worn-down tooth enamel. By relaxing these muscles, jaw botox alleviates these issues. The procedure is performed under local anesthesia and takes approximately 15–30 minutes.
What Are the Benefits of Jaw Botox (Masseter Botox)?
Jaw botox offers both aesthetic and functional benefits. It slims the jawline, giving the face a more balanced appearance. Individuals with a broad or square jawline can achieve a softer, more refined look.
From a functional perspective, jaw botox alleviates issues such as teeth grinding (bruxism) and jaw tension. It reduces pain caused by overactive masseter muscles and helps prevent issues like enamel wear and jaw joint discomfort.
Botox relaxes the masseter muscles, offering relief, especially for those who grind their teeth at night, which also improves sleep quality.
At What Age Can Jaw Botox Be Performed?
Jaw botox is typically suitable for adults. It is approved for individuals aged 18 and older, but for cosmetic purposes, it is recommended that the patient’s facial development be complete, usually by their early twenties. However, if performed to treat functional issues, such as teeth grinding, it can be done at an earlier age.
Botox applications are generally not recommended for younger individuals, as the effects on growing muscles and skin are not fully known. In cases of severe bruxism, doctors may approve this treatment for younger patients, with a carefully planned and monitored treatment process.
How is Gum Botox Done?
Gum botox is a minimally invasive procedure aimed at correcting a gummy smile. The patient first undergoes a thorough examination to identify the muscles causing excessive gum exposure. After local anesthesia is administered to numb the area, botulinum toxin is injected into the upper lip muscles, reducing movement and making the gums less visible.
The procedure usually takes 10–15 minutes, and patients can return to their daily activities immediately. Botox effects are noticeable within 3–4 days and reach full effect in 1–2 weeks, lasting about 3–4 months.
What is the Treatment Process for Jaw Botox for Teeth Grinding?
Jaw botox is an effective method for treating teeth grinding. In this treatment, the condition of the masseter muscles and the severity of teeth grinding are evaluated, followed by local anesthesia and an injection of botulinum toxin into the muscles. The procedure generally takes 15–30 minutes, with patients able to resume normal activities the same day.
Patients may experience mild sensitivity or swelling, which usually subsides within a few days. Effects become noticeable in 1–2 weeks, and patients often report significant relief from jaw pain and discomfort.
How Soon Does Jaw Botox Take Effect?
Jaw botox begins showing effects within 1–2 weeks after application. After the botulinum toxin is injected, it gradually restricts muscle movement, and full relaxation is achieved within this timeframe.
The effects last for 4–6 months, with a marked reduction in symptoms like teeth grinding and jaw tension. Regular botox applications help keep the muscles relaxed over the long term, potentially leading to a lasting reduction in these issues.
Post-Jaw Botox Care Instructions
There are a few important care tips to follow after jaw botox. First, avoid lying down for at least 4 hours after the procedure to ensure that the botox works on the targeted muscles correctly. Additionally, refrain from touching or rubbing the injected area within the first 24 hours.
Avoid exercise and strenuous physical activities for the first 24 hours, as these may affect the botox application. It is also recommended to avoid alcohol, hot showers, and saunas during this period. Follow your doctor’s instructions carefully and consult them if any side effects occur to achieve the best results.
Is Jaw Botox (Masseter Botox) a Permanent Solution?
Jaw botox provides fast and effective relief for issues like teeth grinding and jaw tension but is not a permanent solution. The effects typically last 4–6 months, and muscle activity gradually returns once the effects wear off. For long-term results, repeated sessions are required. With regular applications, however, the muscles can become less active over time, providing lasting relief from problems like teeth grinding.
Frequently Asked Questions About Gum and Jaw Botox (Masseter Botox)
Which Department Performs Gum Botox?
- Dermatology or plastic surgery departments usually perform gum botox. Some trained dentists also offer this service.
Is Jaw Slimming Botox the Same as Jaw Joint Botox?
- No, jaw-slimming botox reduces the masseter muscles to create a slimmer jawline, while jaw joint botox treats joint pain and dysfunction.
Are There Any Side Effects of Jaw Botox?
- Yes, minor side effects like swelling, bruising, pain, or sensitivity may occur but are typically short-lived and temporary.
Is Masseter Botox Permanent?
- No, the effects last about 4–6 months, after which the muscles may regain activity.
Is Jaw Botox Safe?
- Jaw botox is generally safe when performed correctly by an experienced professional. Side effects are usually mild and temporary.
Can Anyone Get Jaw Botox?
- Jaw botox is effective for individuals with overactive masseter muscles but is not recommended for pregnant or breastfeeding individuals or those with certain neurological conditions.
Does Jaw Botox Affect Smiling?
- Typically, jaw botox does not impact smiling; however, if applied improperly, it can alter facial expressions.
Does Chewing Gum Impact Botox?
- Yes, chewing gum can reduce the effectiveness of botox by strengthening the masseter muscles.
What if Botox Affects a Nerve?
- If botox impacts a nerve, it may temporarily reduce nerve function. This is rare and can be avoided with the correct technique.
How Long Does Jaw Slimming Botox Last?
- The effects last 4–6 months, with regular applications necessary for lasting results.
Does Teeth Grinding Botox Change Face Shape?
- Yes, teeth grinding botox reduces the masseter muscles, resulting in a slimmer, more oval face shape.
🦷 What is Dental Implant Surgery? Dental Implant Surgery Prices 2025
An implant serves as a tooth root within a person’s mouth. The simple answer to the question, “What is an implant surgery?” is that it involves the surgical process of extracting a non-functional tooth and placing a screw-like implant into the resulting root space in the jawbone. A prosthetic tooth is then placed on this screw, giving it the appearance of a natural tooth.
Dental implants may be placed to improve speech abilities, restore chewing functions, and address the aesthetic needs of the patient. While implant surgery can seem intimidating for many, procedures performed by specialized surgeons using the latest technology today enable patients to undergo this process more comfortably and result in longer-lasting implants.

How is Implant Surgery Performed in Women?
In women, the implant surgery process can be managed smoothly if the patient is prepared for treatment and the surgeon is skilled in the procedure. Implant surgery is a treatment option for individuals with missing teeth and follows a specific procedure. After evaluating the patient’s dental and jaw structure, the surgeon designs a plan that considers the patient’s preferences.
The procedure is generally carried out under local anesthesia. After the procedure is completed, the healing process begins. During this time, patients must follow their surgeon’s advice to ensure faster recovery and prevent potential complications.
How is Implant Surgery Performed in Men?
The implant surgery process for men is similar to that for women. The procedure for male patients is nearly identical for surgeons. However, there are a few differences. The jaw structure of men and women is distinct. Men's teeth are thicker and more square-shaped, while women's teeth are more rounded and have a thinner, more aesthetic appearance. Surgeons consider gender-specific features to ensure the prosthetic tooth appears more natural.
How is Implant Surgery Performed in Older Adults?
The process used for young and healthy individuals is also applicable to older patients, but special attention is given to factors such as bone density in elderly patients. Existing health issues and medications taken by elderly patients are carefully reviewed to design a safe procedure.
While the surgery is typically performed under local anesthesia, general anesthesia may be used depending on the patient’s health status. The surgeon carefully places the implant into the jawbone, usually completing this process quickly. Recovery time for older patients may be longer compared to younger patients due to age and health status. Once healing is complete, a permanent prosthetic tooth is placed.
How is Dental Implant Surgery Done?
Here is a step-by-step breakdown for those wondering, “How is dental implant surgery performed?”:
- Local anesthesia is administered to the patient. If a tooth extraction is required in the implant area, the tooth root is removed, and the area is cleaned and prepared for the implant.
- A small incision is made in the area where the implant will be placed, and the implant site is drilled with a specialized drill to accommodate the screw.
- The implant is covered with gum tissue and sutured.
- The screw inserted into the jawbone fuses with the bone within 2 to 6 months.
- A temporary prosthetic tooth can be placed based on the patient’s preference.
- Once complete integration with the jawbone is confirmed, the gum is reopened, and a connector piece is placed.
- An impression is taken of this connector piece to design a custom tooth for the patient.
- After the tooth is crafted, it is secured onto the implant with a connector piece known as an abutment.
Post-surgery, patients should attend regular check-ups and follow the surgeon’s instructions during the healing process.
What Are the Risks of Implant Surgery?
Implant surgery is generally considered safe with minimal risks. However, as with any surgical procedure, unexpected and unwanted outcomes may occur. There is a risk of infection, which is common in all surgeries, and surgeons may prescribe antibiotics to minimize this risk.
There is also a risk of damage to the jawbone during implant placement. An improperly placed or incorrectly sized implant may not integrate well with the jawbone, resulting in nerve damage, pain, swelling, and potential allergic reactions.
What Should I Do After Implant Surgery?
There are several post-operative guidelines to follow after implant surgery. Adhering to these rules helps ensure a smoother and healthier recovery after implant surgery.
Firstly, rest after the surgery and avoid heavy exercise for a while. Stick to soft foods for the recommended period, and avoid very hot or very cold drinks.
Pause any smoking and alcohol consumption. Keep your head elevated to reduce swelling. It’s also essential to maintain oral hygiene by brushing your teeth and keeping your mouth clean. However, avoid applying pressure to the implant area, and clean it with the mouthwash recommended by your doctor.
How Long Does It Take to Recover from Implant Surgery?
The recovery time after implant surgery varies depending on the procedure and the individual’s health status. Complete recovery may take several weeks or months due to the complex and multi-stage nature of the surgery.
The fusion process with the bone generally takes around 3 to 6 months, though patients can resume normal activities a few days after the initial procedure. A temporary prosthetic tooth can be placed until a permanent one is attached, extending the treatment and recovery period.
Frequently Asked Questions
How long does implant surgery take?
The duration varies depending on the number of implants, the patient’s health status, and potential complications during the procedure. However, in general, implant surgery takes about 1 to 3 hours to complete. For precise information, a detailed surgery plan should be prepared with the doctor.
How long do dental implants last?
The longevity of implants depends on material quality and how well the patient cares for them. With proper and regular care, dental implants can last for an extended period. With careful planning and attention to oral hygiene, they may even last a lifetime without any issues.
What are the advantages of dental implant surgery?
Your teeth appear very natural, with no sensation of having dentures, enhancing confidence. It is recommended for oral health, is highly durable, and can last for many years.
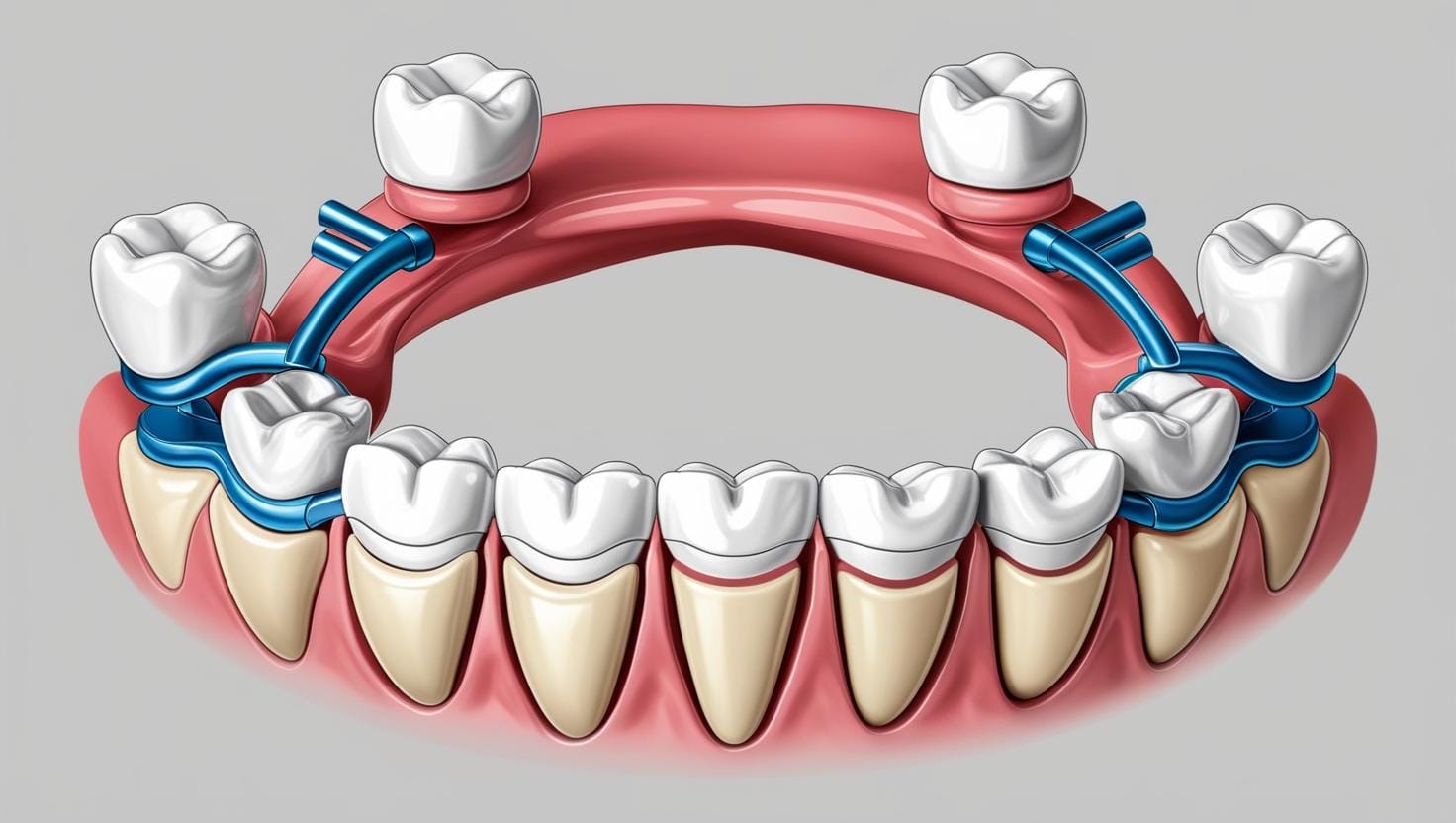
What is a Dental Bridge? How is it Made?
For optimal oral health, it is essential to have healthy teeth. However, in some cases, tooth loss may occur, leading to aesthetic concerns as well as functional issues in speaking and eating. A dental bridge is a method used to treat such cases of tooth loss.
What is a Dental Bridge?
A dental bridge is a type of prosthesis used to replace one or several missing teeth, named for its design that resembles an actual bridge. The structure of a dental bridge consists of one or more artificial teeth that replace missing teeth. The sides of the bridge are prepared to rest on adjacent teeth using crowns that cover those neighboring teeth and secure the bridge in place.
Types of Dental Bridges
Dental bridges can be applied using various methods in oral treatment. Some of the most common types of dental bridges include:
- Traditional Bridges: These types of bridges are used to replace missing teeth and are supported by adjacent teeth. Traditional bridges are stable and durable.
- Cantilever Bridges: Used in cases where there is only one adjacent tooth supporting the bridge. This type of bridge is preferred if tooth loss occurs on only one side.
- Maryland Bridges: These bridges use metal clips or wings to attach to adjacent teeth, requiring less alteration to the tooth structure.
- Implant-Supported Bridges: These bridges rely on implant-supported teeth and are highly durable.

How is a Dental Bridge Made?
The application of a dental bridge involves a multi-step process performed by a dentist. The stages of dental bridge construction include:
- Examination and Preparation: First, the dentist designs and prepares the bridge to replace the missing teeth. The crowns or caps for the adjacent teeth are prepared.
- Taking Measurements: The prepared teeth are measured, and artificial teeth are created in a lab to fit the patient’s mouth structure.
- Temporary Bridge Fitting: While the artificial teeth are being made, the patient may need a temporary bridge. This temporary bridge can reduce aesthetic and functional problems during the waiting period.
- Permanent Bridge Placement: After the artificial teeth are produced and ready, the bridge is permanently placed in the mouth. The crowns covering the neighboring teeth secure the artificial teeth in place.
- Adjustments: Following the placement, the dentist makes necessary adjustments to the bridge to ensure proper biting and chewing functionality.
Advantages and Disadvantages of Dental Bridges
Dental bridges offer several advantages, although there may be a few disadvantages.
Advantages of Dental Bridges:
- Provide aesthetically pleasing results.
- Resolve missing teeth issues and restore chewing function.
- Can improve teeth alignment and spacing.
Disadvantages of Dental Bridges:
- The crowns or caps placed on neighboring teeth may require healthy teeth to be altered.
- The bridge may need replacement over time.
- Less durable than implants.
Who Can Get a Dental Bridge?
Oral health is an essential part of general health, and having healthy teeth positively affects daily life. However, sometimes teeth suffer from damage, loss, or aesthetic issues. Dental bridge treatment is a method used to address such problems by typically creating a bridge anchored to adjacent teeth to support a missing tooth. Recommended cases for dental bridge treatment include:
- Missing Teeth: Dental bridge treatment is used to replace missing teeth, which may result from trauma, decay, or other health issues. Dental bridges support the missing tooth and restore functionality.
- Oral Health: Good gum and tooth health is crucial for dental bridge treatment. Gum infections or severely decayed teeth should be addressed before treatment. A dental bridge should not be applied without treating these issues.
- Oral Hygiene: Maintaining oral hygiene is important after dental bridge treatment. The treated teeth and bridges should be brushed regularly, and dental floss should be used. Otherwise, decay and gum problems may reoccur.
- Healthy Adjacent Teeth: Dental bridge treatment requires strong neighboring teeth. The adjacent teeth support the bridge and bear the force applied during chewing. If there are significant problems with adjacent teeth, these issues may need to be resolved first.
Dental bridge treatment is an effective solution in cases recommended by a dentist. Since each patient's health condition is unique, treatment options vary from person to person.
What to Consider After Dental Bridge Treatment?
After dental bridge treatment, it may be necessary to take some protective measures to ensure the success of the treatment and the longevity of the treated teeth. These protective measures include:
- Regular Oral Hygiene: Following dental bridge treatment, maintaining regular oral hygiene by brushing teeth at least twice daily and using dental floss is essential. Dental bridges are prone to food debris and plaque accumulation, so attention should be given to oral cleanliness.
- Dental Checkups: Regular dental checkups may be required after dental bridge treatment. The dentist can monitor the condition of the bridge and gums and identify potential issues early on. It is generally recommended to have an oral examination twice a year.
- Avoiding Hard Foods: Although dental bridges are durable, excessively hard foods or objects can damage or dislodge the bridge. It may be necessary to avoid such items.
- Managing Teeth Grinding: If a person has a habit of grinding or clenching their teeth, it may be necessary to use a protective splint as recommended by the dentist. Teeth grinding can damage dental bridges.
- Balanced Nutrition: A healthy and balanced diet is important for maintaining general and oral health. Consuming enough calcium and other essential nutrients can strengthen teeth.
- Avoiding Smoking and Alcohol: Smoking and drinking alcohol can lead to gum disease and tooth loss. Such harmful habits should be avoided after dental bridge treatment.
- Protection from Trauma and Accidents: Protecting the mouth and teeth from trauma and accidents is essential for dental health following bridge treatment. Individuals engaging in high-risk sports or activities may need to use a mouthguard.
Taking protective measures after dental bridge treatment can enhance the success of the treatment and prolong the lifespan of the treated teeth. Patients must follow their dentist’s recommendations and instructions. Dental bridge treatment helps individuals regain oral health and achieve an aesthetically pleasing smile.
Frequently Asked Questions About Dental Bridges
Dental bridge treatment is a common choice to replace missing teeth, improve appearance, or restore oral health.
What Are the Costs of a Dental Bridge?
- The dentist examines the patient’s oral health to determine the condition of the teeth, the amount of bridge needed, the number of implants required, and the number of sessions involved. The cost of a dental bridge can vary depending on the treatment plan set by the dentist.
Is a Dental Bridge Procedure Painful?
- Dental bridge treatment is performed under local anesthesia to prevent sensitivity. The patient feels minimal discomfort beyond slight sensitivity.
Dental bridges offer an effective solution for replacing missing teeth. People who need dental bridge treatment should plan their treatment by scheduling an appointment with a dental clinic to restore a healthy oral structure.
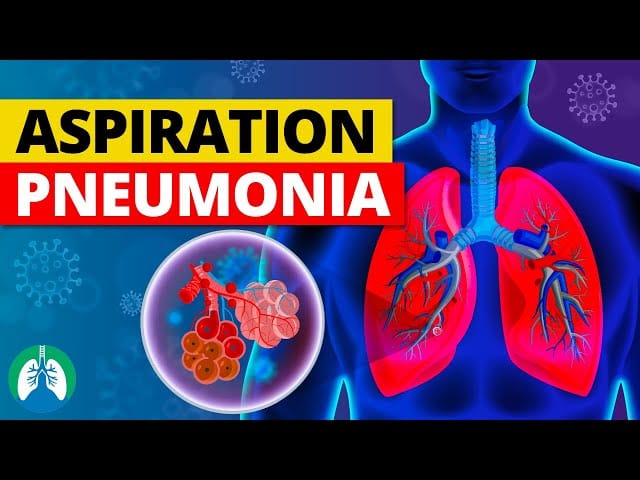
What İs Aspiration Pneumonia?
Aspiration can be defined as the accidental entry of substances intended to reach the stomach into the respiratory tract. These materials, which mistakenly enter the respiratory system during swallowing, can reach the lungs and cause serious complications. Aspiration can occur due to various reasons.
What is Aspiration?
Under normal circumstances, food, saliva, or any other material passes through the pharynx, esophagus, and stomach. On the other hand, air taken through the nose or mouth passes through the pharynx, larynx, trachea, bronchi, and into the lungs. The correct passage of both swallowed substances and air is controlled by a small structure called the epiglottis. During breathing, the epiglottis moves upward, allowing air to pass directly into the larynx. During swallowing, the epiglottis tilts downward, covering the trachea and preventing substances from entering the respiratory tract.
Aspiration occurs when the balance and coordination between swallowing and breathing controlled by the epiglottis are disrupted. In aspiration, materials that should progress to the stomach accidentally enter the trachea, which can have serious health consequences.
Aspiration primarily affects infants, the elderly, and individuals with swallowing disorders. While aspiration may occur without any noticeable symptoms, it can sometimes lead to severe symptoms, such as:
- Feeling of something stuck in the throat
- Pain or difficulty swallowing
- Coughing after eating or drinking
- Sensation of choking while eating
- Making gurgling sounds when swallowing
Additional symptoms that may develop in individuals experiencing aspiration include:
- Excessive saliva in the mouth
- Chest discomfort
- Heartburn
- Fatigue or shortness of breath while eating
- Fever developing shortly after meals (within about 30 minutes)
- Difficulty chewing
- Frequent pneumonia episodes
Aspiration is also common in infants. Some aspiration symptoms in infants are:
- Poor sucking reflex
- Facial redness or grimacing during feeding, with watery eyes
- Rapid or interrupted breathing while feeding
- Mild fever after feeding
- Wheezing and other respiratory problems
- Frequent respiratory infections or pneumonia
What Causes Aspiration?
Aspiration can develop for different reasons in adults and infants.
Causes of Aspiration in Adults
The primary cause of aspiration in adults is impaired swallowing function. When swallowing does not occur normally, the mechanisms preventing aspiration may fail, leading to substances entering the respiratory tract. The main causes of aspiration in adults include:
- Loss of Tongue Control: The tongue is a muscular organ controlled by nerves. Loss or weakening of this control can impair the swallowing reflex, leading to aspiration, especially of liquids.
- Abnormal Swallowing Reflex: A dysfunctional swallowing reflex allows food or other materials to enter the airway.
- Neurological Diseases: Conditions like Parkinson’s disease can impair tongue control and cause aspiration.
- Esophageal Disorders: Problems with the esophagus, such as gastroesophageal reflux disease (GERD), dysphagia (painful swallowing), or throat cancer, can contribute to aspiration.
- Neck Surgery: Surgical procedures affecting the larynx can disrupt swallowing. If the epiglottis is damaged, the coordination between breathing and swallowing may be compromised.
- Oral and Dental Problems: Dental issues can impair chewing and swallowing, increasing the risk of aspiration.
- General Anesthesia: During surgeries, the contents of the stomach may flow back into the respiratory tract, posing a risk of aspiration. Surgical teams take precautions to prevent this by requiring patients to fast before procedures.
Causes of Aspiration in Infants
In infants, aspiration often occurs due to swallowing dysfunction related to issues with the throat muscles. Conditions that may weaken the throat muscles in infants include:
- Physical abnormalities like cleft palate
- Growth retardation
- Brain damage
- Nerve damage
- Neuromuscular disorders such as cerebral palsy or spinal muscular atrophy
What Are the Complications of Aspiration?
Aspirating solid or liquid substances can lead to serious health problems.
Aspiration Complications in Adults
Aspiration can result in severe issues, including infections and tissue damage. One of the most serious complications is aspiration pneumonia, which occurs when materials entering the lungs cause an infection. Aspiration pneumonia leads to inflammation and fluid accumulation in the lungs. Its symptoms may develop slowly over time and include:
- Frequent coughing with foul-smelling sputum
- Shortness of breath
- Fever, sweating, and chills
- Chest pain or the need to cough when taking deep breaths
- Anxiety, fatigue, or confusion
- Feeling of suffocation
Aspiration Complications in Infants
In infants, aspiration can lead to similar complications, including pneumonia. Additionally, chronic aspiration may result in dehydration, malnutrition, and weight loss.
How is Aspiration Diagnosed and Treated?
Early diagnosis and treatment of aspiration are crucial to prevent complications.
Diagnosis
If aspiration causes noticeable symptoms, it becomes easier to detect and diagnose. However, in some cases, symptoms may not be obvious, making diagnosis more challenging. The diagnostic process usually involves a patient interview and physical examination. The following methods may be used to diagnose aspiration:
- X-rays: These help assess the effectiveness of breathing.
- Bronchoscopy: A thin tube with a camera is inserted into the respiratory tract to view the inside of the lungs.
- Modified Barium Swallow Test: The patient swallows liquids or solids containing barium, and a series of images are taken to check for leaks into the airway.
- Fiberoptic Endoscopic Evaluation of Swallowing (FEES): A thin tube with a camera is inserted through the nose to view the throat and larynx while the patient swallows saliva or food. This helps detect any leakage into the airway.
Treatment
The primary aim of aspiration treatment is to address the underlying cause. Without resolving the root issue, eliminating aspiration completely may not be possible.
Some measures to prevent aspiration include:
- Eating small bites of food
- Remaining calm and relaxed while eating
- Softening dry foods with sauces or liquids
- Avoiding taking new bites before swallowing the previous one
- Refraining from talking while eating or drinking
- Avoiding eating or drinking while lying down
- Maintaining good oral and dental hygiene
- Avoiding smoking
Aspiration can lead to serious health problems in both adults and infants. To prevent these issues, necessary precautions should be taken during feeding. Individuals experiencing symptoms of aspiration should seek medical attention promptly. Stay healthy!
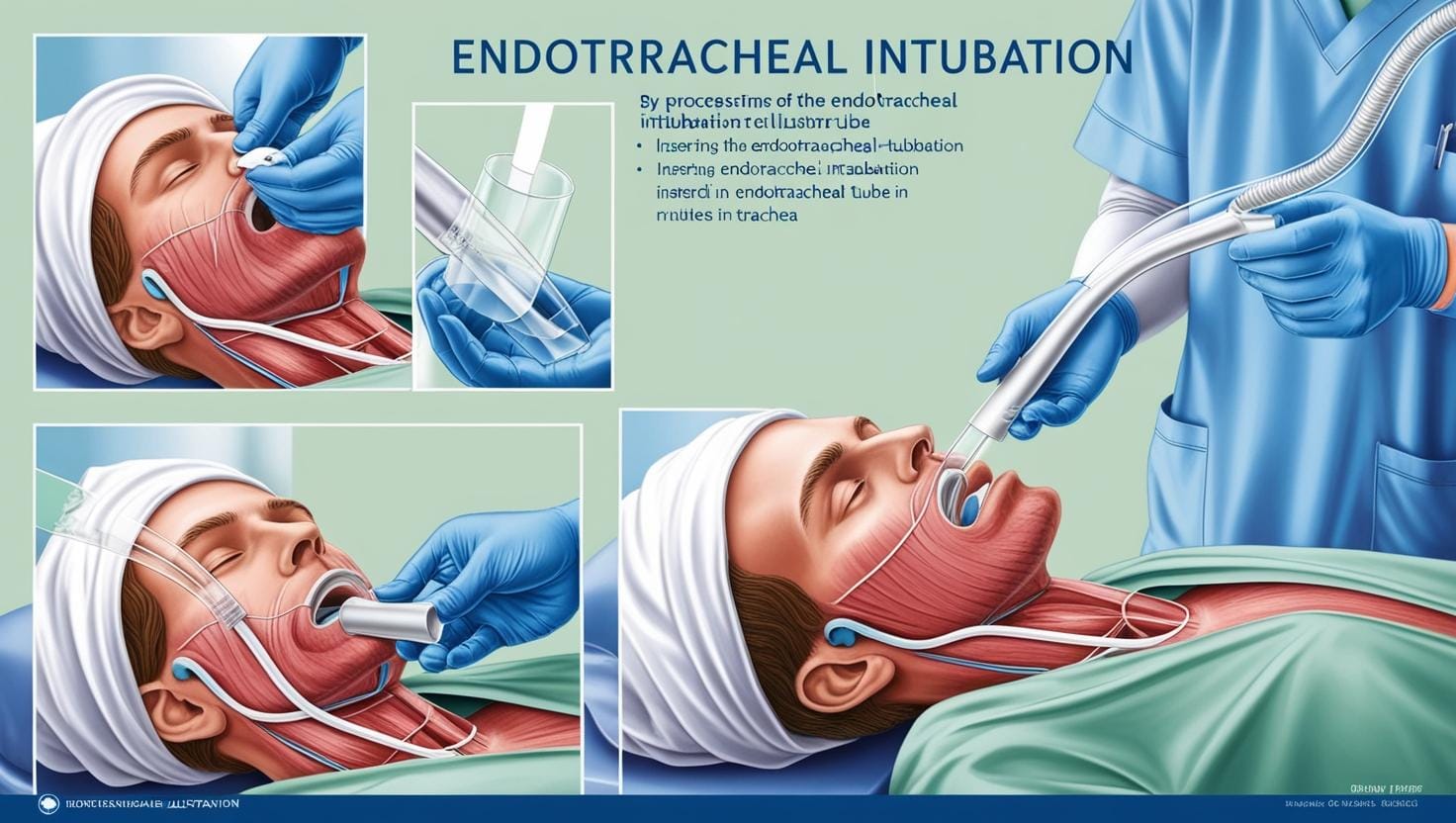
What is intubation? How is Intubation Done?
Intubation involves the insertion of a thin tube, called an endotracheal tube, through the mouth into the airway. This procedure connects the patient to a ventilator, a device that assists or takes over the process of breathing. Intubation is performed in situations where the patient requires anesthesia, sedation, or respiratory support due to a severe medical condition. It is a common medical practice today for maintaining adequate oxygen supply and airway control.
What Does "Being Intubated" Mean?
The term “intubated patient” has become widely recognized, prompting questions such as, “What does intubation mean, and why are patients intubated?” An intubated patient refers to someone who has undergone the intubation process to receive respiratory support. This is usually necessary for individuals who cannot manage their airways or breathe unassisted.
Why is Intubation Necessary?
Patients may require intubation during surgeries, especially under general anesthesia, since the drugs used affect all muscles, including the diaphragm, making independent breathing impossible. In most cases, the endotracheal tube is removed after surgery when the anesthesia wears off, allowing the patient to resume normal breathing.
However, in cases involving major surgeries like open-heart procedures or serious respiratory conditions, the tube may remain in place longer, with the patient breathing through a ventilator.
Intubation is also required in cases of respiratory failure caused by conditions such as:
- Severe lung injury
- Pneumonia
- COVID-19
How is Intubation Performed?
Before the procedure, the patient is typically under anesthesia or sedation, or unconscious due to illness, which facilitates easier access to the airway. The patient is laid flat on their back, and the clinician, positioned at the patient’s head, gently opens the mouth and advances a tube using a tool equipped with light. Pressure is applied to the tongue to prevent airway obstruction, and the tube is carefully inserted into the airway. To confirm proper placement, the clinician listens to the patient’s lungs using a stethoscope.
In some cases, nasal intubation (using a nasotracheal tube) may be performed, especially when oral access is restricted. Pediatric intubation follows the same principles but requires smaller instruments due to children’s narrower airways.
Extubation and Recovery
Once the patient no longer needs intubation, the tube is removed through a process called extubation. The balloon securing the tube is deflated, and the tube is gently withdrawn. The patient is then closely monitored for any respiratory distress, which may necessitate additional oxygen support.
Risks of Intubation
While intubation is often necessary to save lives, it carries some risks, especially if the procedure is prolonged:
- Injuries to the teeth, tongue, throat, or larynx
- Insertion of the tube into the esophagus instead of the trachea
- Tracheal injury
- Bleeding or aspiration (inhalation of fluids or food into the lungs)
- Pneumonia or lung infections
Nutrition During Intubation
For short procedures, no special feeding is required, but for extended intubation, nutrition is provided via intravenous (IV) fluids or a feeding tube. Feeding can be done using orogastric (through the mouth) or nasogastric (through the nose) tubes. These methods ensure that the patient receives necessary nutrients while intubated.
Intubation, despite its risks, is a critical medical procedure, often used to address respiratory issues caused by diseases like pneumonia, COVID-19, or chronic obstructive pulmonary disease (COPD). It ensures that patients in respiratory distress receive adequate oxygen and airway management, essential for survival in severe cases.
What are Intestinal Diseases?
Definition of Inflammatory Bowel Disease: Inflammatory bowel diseases are a term used for diseases that result from chronic inflammation in the digestive system, primarily affecting the intestines. The two most common types of inflammatory bowel diseases are ulcerative colitis and Crohn's disease.
Ulcerative Colitis: This condition primarily affects the colon and rectum. In ulcerative colitis, the superficial layer that lines the colon is affected, leading to the formation of ulcers on the intestinal surface.
Crohn's Disease: Crohn's disease can affect any part of the digestive system, but it most frequently involves the small intestine. While only the surface layer of the intestine is affected in ulcerative colitis, deeper tissues can be affected in Crohn's disease.
The symptoms of inflammatory bowel diseases vary depending on the area affected and the severity of the inflammation. Some patients may exhibit milder symptoms, while others may experience severe indications. Inflammatory bowel diseases can manifest with flare-ups when symptoms intensify and remission periods when symptoms subside. Common symptoms in ulcerative colitis and Crohn's disease include:
- Diarrhea
- Abdominal pain
- Blood in stool
- Abdominal cramps
- Loss of appetite
- Fatigue and weakness
- Unintentional weight loss
Individuals showing one or more of these symptoms or noticing changes in their bowel movements recently should consult a doctor for necessary examinations. As inflammatory bowel diseases can lead to serious health issues, their diagnosis and treatment should not be overlooked.
What are the Complications of Inflammatory Bowel Diseases?
Inflammatory bowel diseases can lead to some undesirable effects in the body. Common complications that can occur in both ulcerative colitis and Crohn's disease include:
- Colon Cancer: Patients whose large intestine has been significantly affected by ulcerative colitis or Crohn's disease have an increased risk of developing colon cancer. Patients diagnosed with inflammatory bowel cancer begin screening for colon cancer 8-10 years after diagnosis. The timing of the screening may vary based on the patient's age, comorbidities, and family history, so diagnosed patients should discuss when to start screening with their doctor.
- Skin, Eye, and Joint Inflammations: During flare-ups of inflammatory bowel diseases, conditions like arthritis (joint inflammation), skin lesions, and uveitis may occur.
- Medication Side Effects: Some medications used to treat inflammatory bowel diseases may carry a slight risk of cancer development. Corticosteroids used in treatment can also lead to conditions such as osteoporosis and high blood pressure.
- Primary Sclerosing Cholangitis: This condition, which involves the inflammation and narrowing of the bile ducts within the liver, can lead to impaired liver function. People with primary sclerosing cholangitis are likely to have inflammatory bowel disease.
- Blood Clots: Inflammatory bowel diseases increase the risk of blood clot formation within blood vessels.
Undesirable Conditions Associated with Crohn's Disease:
- Intestinal Obstruction: Crohn's disease can affect all layers of the intestinal wall, causing the affected segment to thicken and narrow, obstructing the passage of digestive materials through the intestine.
- Malnutrition: Patients with Crohn's may struggle to eat due to diarrhea, abdominal pain, and cramps. Additionally, absorption issues may occur in the intestine, leading to insufficient intake of essential nutrients. This can result in vitamin B12 and iron deficiency anemia.
- Fistula Formation: A fistula refers to an abnormal connection between two different parts of the body. In Crohn's disease, inflammation of the intestinal wall can lead to the formation of fistulas connecting to other organ walls, most commonly occurring in the anal region. A fistula may become infected and form an abscess.
- Anal Fissure: Patients with Crohn's may develop small tears in the skin around the anus, known as anal fissures.
Complications Seen in Ulcerative Colitis:
- Toxic Megacolon: In patients with ulcerative colitis, the colon may suddenly swell and expand, leading to a condition called toxic megacolon.
- Intestinal Perforation: Toxic megacolon can cause intestinal perforation, which can occur spontaneously.
- Severe Fluid Loss: Excessive fluid loss due to diarrhea can lead to dehydration.
What Causes Inflammatory Bowel Diseases?
The exact causes of inflammatory bowel diseases remain unclear. Experts believe that various factors, including diet, genetics, stress, and environmental factors, may play a role in disease development.
The immune system also plays a role in the development of inflammatory bowel diseases. Under normal circumstances, the immune system recognizes and destroys harmful microorganisms such as bacteria, viruses, and parasites that enter the digestive system. During this process, inflammation occurs in the intestine to combat the infection. Once the infection is resolved, the inflammation subsides, and the intestine returns to its normal state. In healthy individuals, the infection process operates in this manner. However, in inflammatory bowel diseases, inflammation occurs in the absence of an infection. The immune system attacks the healthy intestinal cells, leading to organ damage.
Risk Factors for Inflammatory Bowel Diseases:
- Age: Patients diagnosed with inflammatory bowel diseases are often under 30, though some may not develop the disease until their 50s.
- Family History: Individuals with first-degree relatives (parents, siblings, children) who have inflammatory bowel diseases are at a higher risk.
- Smoking: Smoking is the most significant controllable risk factor for developing Crohn's disease.
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Medications containing active ingredients like ibuprofen, naproxen sodium, and diclofenac sodium pose risks for both the development of the disease and the progression of existing conditions.
Diagnosis and Treatment of Inflammatory Bowel Diseases:
Diagnosis involves a comprehensive investigation considering other disorders that could cause similar symptoms and signs. Blood tests and stool tests are performed to evaluate potential diseases. Endoscopy and colonoscopy are used to assess the effects of ulcerative colitis or Crohn's disease on the digestive organs. For patients with conditions like intestinal perforation where endoscopic methods cannot be applied, imaging methods such as X-ray, CT, or MRI may be utilized.
The primary goal in treating inflammatory bowel diseases is to reduce the inflammation causing the disorder. Reducing inflammation alleviates both symptoms and signs, contributing to long-term remission of the disease. Additionally, treatment can help prevent complications that may arise from the disease.
Both medication and surgical methods can be employed in treatment.
In Medication Treatment:
- Anti-inflammatory medications such as corticosteroids to reduce inflammation.
- Immunosuppressive drugs like azathioprine and methotrexate to suppress the immune response.
- Antibiotics may be used if an infection develops due to the disease.
- Depending on the patient's condition, the doctor may prescribe anti-diarrheal, pain relief medications, and vitamin supplements.
When significant weight loss occurs or nutritional intake severely declines in patients with inflammatory bowel disease, nutritional support may be initiated. Specialized nutritional methods, such as tube (enteral nutrition) or intravenous nutrition (parenteral nutrition), may be implemented to facilitate recovery and rest the intestine.
In the surgical treatment of ulcerative colitis and Crohn's disease, the affected section of the intestine is removed, allowing the remaining intestine to function healthily. Surgical intervention may also be necessary for complications such as intestinal obstruction. However, surgery does not provide a definitive solution for these diseases. The operation is performed to improve the patient's overall condition and prevent possible complications.
If you suspect you have inflammatory bowel disease, consult a qualified healthcare facility for necessary examinations. It is beneficial for individuals diagnosed with inflammatory bowel disease to consult a gastroenterologist to discuss the most effective treatment methods and obtain detailed information about the disease.
Wishing you healthy days.