What is Jaw Prosthesis? Types of Jaw Prosthesis
A jaw prosthesis is a special prosthetic used to repair or reconstruct the missing tip or jawbone area. These prostheses significantly improve your facial aesthetics by defining your facial features. In addition to aesthetic concerns, prostheses also support chewing functions, enhancing daily comfort. So, how is a jaw prosthesis made, and what are the things you should know about it?
What is Jaw Prosthesis?

Jaw prostheses are specially designed according to your individual needs. Each patient has a different jaw size and shape, so the prosthesis is customized to fit you perfectly. Typically made from biocompatible materials, these prostheses are created from materials like silicone, polyurethane, or acrylic.
The choice of material offers both aesthetic and functional advantages. The prosthesis is secured using screws placed in the bone behind your teeth or through bands, ensuring it remains stable even during chewing and can be safely used.
Jaw prostheses are also used in cases of trauma or to reconstruct jaw tips lost due to some types of cancer. They can improve the jaw size in cases of aging, tooth loss, or other health problems. Additionally, enhanced chewing abilities can positively impact your general dietary habits. It is an excellent option to correct aesthetic appearance and strengthen jaw structure. Unlike temporary fillings, jaw prostheses provide a permanent solution for long-lasting satisfaction.
What are the Types of Jaw Prosthesis?
There are special implants used for treating deficiencies or deformities in the oral region. They are typically used in cases of tooth loss, fractures, trauma, tumors, or congenital anomalies. They are designed to correct structural issues.
These prostheses come in various types depending on the material used. Materials like titanium, acrylic, porcelain, and rubber are preferred to increase the durability and longevity of the prosthesis.
Why are Jaw Prostheses Needed?
A jaw prosthesis is a significant consideration for many individuals concerned with facial aesthetics and proportions. If your jaw appears small, recessed, or weak, it can cause feelings of insecurity. A jaw implant surgery offers the chance to solve these issues and improve your self-confidence.
The benefits of jaw prostheses include making your jaw more proportionate with your face, improving the overall facial harmony. You can achieve a more symmetrical face with the help of these implants. Correcting a weak or recessed jaw is another important advantage of the prosthesis. Such a transformation not only affects your appearance but also your manner of expression.
With more defined features, your other facial traits stand out, and the overall balance improves. The implant also enhances your neck and jawline, resulting in a more prominent and aesthetic appearance.
A small bone structure can eventually lead to an aged or dual look, but a jaw prosthesis can significantly improve your aesthetics and psychological well-being.
When Should a Jaw Prosthesis Be Used?
A jaw prosthesis may be considered when you experience restricted jaw movement, signs of joint stiffness, or jaw pain. In such cases, it is essential to try other treatments before resorting to surgery.
If you have previously undergone surgery and it was unsuccessful, you may need reconstructive surgery. In these situations, a jaw prosthesis is evaluated as the most appropriate solution. Congenital disorders also require implants.
Some individuals are born with joint problems that become more pronounced with age. If you are experiencing such a condition, it is helpful to consult with an expert to clarify your situation.
A jaw prosthesis should be considered as a last resort in TMJ (temporomandibular joint) treatment. Therefore, you should also consider other treatment methods recommended by your specialist.
It is an effective treatment for patients with TMJ damage. There are various conditions that can lead to permanent damage in the joint, such as trauma or arthritis. Joint damage significantly affects daily life and must be treated by surgical specialists, who aim to improve quality of life.
What to Do After Jaw Prosthesis Surgery?
There are some important rules to follow after jaw prosthesis surgery to ensure a smooth recovery and protect your health.
- To prevent infection after the surgery, it is important to avoid harmful products for the first 4 months.
- In the first week, take showers while sitting down and spend a maximum of 10 minutes in lukewarm water.
- Unless otherwise advised by your doctor, avoid solid foods for 4-6 weeks after the surgery.
- Stay away from herbal teas, and especially from summer fruits like strawberries and cherries.
- Be gentle while brushing your teeth to avoid damaging the stitches inside your mouth. Move slowly while performing oral hygiene.
- Continue taking the prescribed medications as directed by your doctor. It is important not to skip doses to manage pain and discomfort.
- Avoid hot drinks as your stitches inside the mouth have not healed.
- If you notice any signs of infection during the recovery period, consult your doctor immediately.
Frequently Asked Questions
What is the Disability Rate for Jaw Prosthesis?
The disability rate caused by jaw prosthesis can vary depending on several factors. The material used for the prosthesis and the reason for the procedure both affect the disability rate. You can get more detailed information about the disability rate from hospitals.
How Much Do Jaw Prostheses Cost?
The cost of jaw prostheses varies depending on several factors. Primarily, the patient's individual needs and aesthetic expectations significantly influence the cost. Since each person's jaw and face shape are different, the material and techniques used by the surgeon also impact the price. Additionally, the location of the clinic or hospital can affect the price.
How Often Should a Jaw Prosthesis Be Replaced?
This depends on the condition of the jaw prosthesis and the overall oral health. Typically, the durability lasts between 5 to 10 years, but it can vary based on changes in jaw structure, usage, and maintenance. Partial prostheses, however, can last up to 15 years on average.
How to Maintain Jaw Prosthesis?
Proper maintenance is crucial to protect your oral and jaw health and extend the lifespan of your implant. The first step is to clean the prosthesis daily. Additionally, it is recommended to use cleaning tablets for deep cleaning once a week. During the cleaning process, ensure that the prosthesis is not at risk of falling and breaking. To minimize the risk, it is advised to perform cleaning near a water-filled basin.
What is Tooth Root Resection? Tooth Root Resection Treatment
Root resection is a procedure performed on the tooth root, typically when an infection or lesion develops within the root area due to oral health issues. In cases where infection or lesions are present, surgical intervention is necessary to clean the affected area and preserve oral health.
The procedure involves partial or complete removal of the tooth root to eliminate the infection. Before the resection, any existing infection must be controlled to prevent its spread. Through this method, infected tissues and lesions are removed, a process known as root resection.
Early intervention is crucial if any discomfort arises in the root, as untreated root infections can lead to tooth loss. Prompt treatment not only protects the affected tooth but also shortens the healing process.
Types of Root Resection

There are several methods based on the spread and nature of the infection or lesion:
- Benign Lesions: These do not spread to adjacent roots and are often treated with simple procedures, such as root canal therapy.
- Aggressive Infections: If infection spreads to neighboring tooth roots, antibiotics are typically prescribed to control inflammation before resection.
Diagnosis of Root Resection
Physical examination, often supplemented with imaging techniques, helps to assess the root condition, lesion size, and infection severity. X-rays reveal critical details, aiding the dentist in tailoring the treatment.
Treatment for Root Resection
The initial step is to identify the infection source, enabling a more targeted treatment approach. Antibiotics may be administered to control the infection, preparing the area for surgical intervention.
Root Resection Surgery
The area is numbed with local anesthesia, allowing the dentist to access the affected root area and clean the infected tissue. A small filling may be placed over the cleaned area. Surgery duration depends on the infection’s severity and lesion size.
Post-Root Resection Recovery
Maintaining oral hygiene post-surgery is essential to prevent recurring infections. Dentists advise patients to avoid consuming solid or hot foods until numbness subsides and avoid smoking to reduce complications.
Key steps during recovery:
- Avoid physical activity for a week to prevent bleeding risks.
- Apply cold compresses intermittently to reduce swelling.
- Ensure stitches are kept untouched to avoid damage.
Stitches are usually removed within 7-10 days, with periodic checkups between 3-6 months to monitor healing progress.
FAQs About Root Resection
Is Root Resection Dangerous?
No, it is a minimally invasive procedure aimed at treating infected root areas without compromising the tooth structure.
Is Root Resection Cancerous?
No, root resection treats infections and lesions, not cancerous growths. The procedure is focused on removing inflamed or infected tissues to alleviate discomfort.
How is a Root Resection Cleaned?
Under local anesthesia, a small incision is made to access and clean the infected root tissue, completing the resection procedure efficiently.
This content is optimized to provide accurate information on root resection treatment for better search engine visibility and readability.
How is Apical Resection Surgery Performed?
Apical resection surgery is a surgical method used to treat lesions that develop in tooth roots. When root canal treatment is insufficient, the inflamed part of the tooth root can be treated using this method. Apical resection becomes necessary when lesions in the tooth root advance to a stage requiring surgical intervention. It is particularly useful for removing advanced infections from the tooth root through surgery.
Types of Apical Resection

Apical resection surgery is not always necessary. Generally, it is preferred when lesions in the tooth root reach an advanced stage. Here is a summary of types of dental lesions that may require apical resection surgery:
- Tooth Decay: Decay in the teeth can erode the tooth enamel over time, potentially reaching the root, which may require surgery if not controlled.
- Tooth Fracture: Excessive force or environmental factors can cause tooth fractures, leading to pain and sensitivity.
- Damage to Tooth Enamel: Frequent consumption of acidic foods or using a hard-bristled toothbrush can damage and sensitize the tooth enamel over time.
- Dental Cyst: Cysts that form at the tip of the tooth root often require surgical intervention.
How is Apical Resection Diagnosed?
Unhealthy eating habits and inadequate oral and dental care can lead to the growth of oral bacteria over time. These bacteria can accumulate in decayed teeth, extending to the root and causing various infections. When the infection progresses, root canal treatment may be insufficient, requiring surgical removal of the infection.
Apical resection surgery is used in cases where lesions cause other significant effects over time. During dental examinations, the presence of the following factors may indicate the need for apical resection:
- A lesion in the tooth root has damaged the root.
- Benign cyst formation has occurred in the tooth root.
- The infection affects the front teeth.
- Root canal treatment was unsuccessful, or pain continues after the procedure.
- Structural abnormalities in the root or jaw prevent successful root canal treatment.
- The infected tooth root is pressing on other tooth roots.
How is Apical Resection Treated?
Apical resection is a surgical procedure. If not performed when necessary, it may cause swelling or other infections in the tooth root. Issues in the tooth root may sometimes be treated with root canal therapy, but advanced cases may require surgery. The suitability of surgery is primarily determined based on the existing conditions, which are assessed to initiate treatment.
During apical resection, infected tissue at the tooth root and surrounding areas are exposed. The infected root canals are cleaned of bacteria and infections, allowing the tooth to regain its previous function. The treatment is completed by sealing the tooth. Since the procedure is performed under anesthesia, it is painless and typically takes 30-90 minutes, depending on the structure of the tooth.
Why is Apical Resection Performed?
Apical resection is critical to preserving the structure of the tooth root without removal. The method treats lesions in the tooth root, preserving the tooth structure. The primary benefits of apical resection treatment include:
- Treating infection in the tooth root, preventing tooth loss.
- Restoring the tooth’s previous function.
- Alleviating pain and discomfort caused by lesions.
- Preventing the infection from spreading to surrounding tissues.
Apical Resection Surgery
When a specialist identifies advanced infections, they may examine the condition of the infected tooth with an x-ray. If the infection is suitable for surgery, treatment may begin. To prevent infection progression before the procedure, the patient may need to take antibiotics. The following are the steps involved in apical resection surgery:
- The infected tooth root and surrounding areas are numbed with local anesthesia.
- A small incision is made in the tissue to access the infected area.
- Part of the tooth root and surrounding infected tissue is removed.
- The cleaned root canals are sealed to prevent further lesion formation.
- After disinfection, the gum tissue is sutured, and the procedure is completed.
Following the procedure, the healing of the tooth root is monitored. X-rays may be used to observe the formation of new bone around the root, indicating recovery and a successful outcome.
Post-Procedure Healing Process
The healing process after apical resection may vary for each individual. Pain or minor bleeding may occur during recovery, and painkillers may be prescribed. Patients can also take additional measures to support healing:
- Applying an ice pack in the first 10-12 hours can reduce pain.
- Using medications prescribed by the specialist to manage pain, swelling, or bruising.
- Maintaining good oral hygiene and avoiding acidic foods.
- Avoiding very hot or cold foods.
- Using a soft toothbrush and mouthwash for gentle care.
These precautions significantly affect the healing process, alongside regular follow-up visits to the specialist.
Frequently Asked Questions
Is Apical Resection Dangerous?
Although apical resection surgery is a painless procedure, some complications may occur, such as swelling, bruising, minor bleeding, or wounds in the affected area. While most of these resolve over time, some may be permanent.
Is Apical Resection Cancerous?
Infections in the tooth root are usually benign, rarely posing a cancer risk. Most benign lesions can be treated with apical resection surgery and heal quickly. However, malignant lesions, though rare, should be closely monitored by a specialist.
How is Apical Resection Cleaned?
If root canal treatment fails, surgical intervention is essential to remove the infected tissue and restore the tooth's function.
What is Gum Botox and Jaw Botox (Masseter Botox)?
Gum botox and jaw botox (masseter botox) have become popular in recent years for both aesthetic and functional purposes. These types of botox are used to enhance gum appearance and relax jaw muscles.
What is Gum Botox?
Gum botox is a cosmetic procedure designed to prevent excessive gum exposure during smiling. Some individuals find that too much of their gum tissue shows when they smile, a concern known as a gummy smile. To address this, botulinum toxin (botox) is injected into the upper lip muscles, reducing the visibility of the gums and creating a more balanced smile.
This procedure is minimally invasive, with quick recovery and a short treatment time. Performed under local anesthesia, gum botox typically lasts 3–4 months and can be repeated as needed. When administered correctly, it provides a natural, pleasant smile, making it a safe and effective option.
What is Jaw Botox (Masseter Botox)?
Jaw botox, also known as masseter botox, is a cosmetic and functional procedure in which botulinum toxin is injected into the masseter muscles.
These muscles are primarily responsible for chewing, and in some cases, they may become overactive, resulting in a wider jawline, square facial structure, or teeth grinding (bruxism). Jaw botox helps by reducing the activity of these muscles, creating a slimmer jawline and a more oval face shape.
It is also an effective treatment for teeth grinding and jaw tension. Overactive masseter muscles can lead to jaw pain, headaches, and worn-down tooth enamel. By relaxing these muscles, jaw botox alleviates these issues. The procedure is performed under local anesthesia and takes approximately 15–30 minutes.
What Are the Benefits of Jaw Botox (Masseter Botox)?
Jaw botox offers both aesthetic and functional benefits. It slims the jawline, giving the face a more balanced appearance. Individuals with a broad or square jawline can achieve a softer, more refined look.
From a functional perspective, jaw botox alleviates issues such as teeth grinding (bruxism) and jaw tension. It reduces pain caused by overactive masseter muscles and helps prevent issues like enamel wear and jaw joint discomfort.
Botox relaxes the masseter muscles, offering relief, especially for those who grind their teeth at night, which also improves sleep quality.
At What Age Can Jaw Botox Be Performed?
Jaw botox is typically suitable for adults. It is approved for individuals aged 18 and older, but for cosmetic purposes, it is recommended that the patient’s facial development be complete, usually by their early twenties. However, if performed to treat functional issues, such as teeth grinding, it can be done at an earlier age.
Botox applications are generally not recommended for younger individuals, as the effects on growing muscles and skin are not fully known. In cases of severe bruxism, doctors may approve this treatment for younger patients, with a carefully planned and monitored treatment process.
How is Gum Botox Done?
Gum botox is a minimally invasive procedure aimed at correcting a gummy smile. The patient first undergoes a thorough examination to identify the muscles causing excessive gum exposure. After local anesthesia is administered to numb the area, botulinum toxin is injected into the upper lip muscles, reducing movement and making the gums less visible.
The procedure usually takes 10–15 minutes, and patients can return to their daily activities immediately. Botox effects are noticeable within 3–4 days and reach full effect in 1–2 weeks, lasting about 3–4 months.
What is the Treatment Process for Jaw Botox for Teeth Grinding?
Jaw botox is an effective method for treating teeth grinding. In this treatment, the condition of the masseter muscles and the severity of teeth grinding are evaluated, followed by local anesthesia and an injection of botulinum toxin into the muscles. The procedure generally takes 15–30 minutes, with patients able to resume normal activities the same day.
Patients may experience mild sensitivity or swelling, which usually subsides within a few days. Effects become noticeable in 1–2 weeks, and patients often report significant relief from jaw pain and discomfort.
How Soon Does Jaw Botox Take Effect?
Jaw botox begins showing effects within 1–2 weeks after application. After the botulinum toxin is injected, it gradually restricts muscle movement, and full relaxation is achieved within this timeframe.
The effects last for 4–6 months, with a marked reduction in symptoms like teeth grinding and jaw tension. Regular botox applications help keep the muscles relaxed over the long term, potentially leading to a lasting reduction in these issues.
Post-Jaw Botox Care Instructions
There are a few important care tips to follow after jaw botox. First, avoid lying down for at least 4 hours after the procedure to ensure that the botox works on the targeted muscles correctly. Additionally, refrain from touching or rubbing the injected area within the first 24 hours.
Avoid exercise and strenuous physical activities for the first 24 hours, as these may affect the botox application. It is also recommended to avoid alcohol, hot showers, and saunas during this period. Follow your doctor’s instructions carefully and consult them if any side effects occur to achieve the best results.
Is Jaw Botox (Masseter Botox) a Permanent Solution?
Jaw botox provides fast and effective relief for issues like teeth grinding and jaw tension but is not a permanent solution. The effects typically last 4–6 months, and muscle activity gradually returns once the effects wear off. For long-term results, repeated sessions are required. With regular applications, however, the muscles can become less active over time, providing lasting relief from problems like teeth grinding.
Frequently Asked Questions About Gum and Jaw Botox (Masseter Botox)
Which Department Performs Gum Botox?
- Dermatology or plastic surgery departments usually perform gum botox. Some trained dentists also offer this service.
Is Jaw Slimming Botox the Same as Jaw Joint Botox?
- No, jaw-slimming botox reduces the masseter muscles to create a slimmer jawline, while jaw joint botox treats joint pain and dysfunction.
Are There Any Side Effects of Jaw Botox?
- Yes, minor side effects like swelling, bruising, pain, or sensitivity may occur but are typically short-lived and temporary.
Is Masseter Botox Permanent?
- No, the effects last about 4–6 months, after which the muscles may regain activity.
Is Jaw Botox Safe?
- Jaw botox is generally safe when performed correctly by an experienced professional. Side effects are usually mild and temporary.
Can Anyone Get Jaw Botox?
- Jaw botox is effective for individuals with overactive masseter muscles but is not recommended for pregnant or breastfeeding individuals or those with certain neurological conditions.
Does Jaw Botox Affect Smiling?
- Typically, jaw botox does not impact smiling; however, if applied improperly, it can alter facial expressions.
Does Chewing Gum Impact Botox?
- Yes, chewing gum can reduce the effectiveness of botox by strengthening the masseter muscles.
What if Botox Affects a Nerve?
- If botox impacts a nerve, it may temporarily reduce nerve function. This is rare and can be avoided with the correct technique.
How Long Does Jaw Slimming Botox Last?
- The effects last 4–6 months, with regular applications necessary for lasting results.
Does Teeth Grinding Botox Change Face Shape?
- Yes, teeth grinding botox reduces the masseter muscles, resulting in a slimmer, more oval face shape.
🦷 What is Dental Implant Surgery? Dental Implant Surgery Prices 2025
An implant serves as a tooth root within a person’s mouth. The simple answer to the question, “What is an implant surgery?” is that it involves the surgical process of extracting a non-functional tooth and placing a screw-like implant into the resulting root space in the jawbone. A prosthetic tooth is then placed on this screw, giving it the appearance of a natural tooth.
Dental implants may be placed to improve speech abilities, restore chewing functions, and address the aesthetic needs of the patient. While implant surgery can seem intimidating for many, procedures performed by specialized surgeons using the latest technology today enable patients to undergo this process more comfortably and result in longer-lasting implants.

How is Implant Surgery Performed in Women?
In women, the implant surgery process can be managed smoothly if the patient is prepared for treatment and the surgeon is skilled in the procedure. Implant surgery is a treatment option for individuals with missing teeth and follows a specific procedure. After evaluating the patient’s dental and jaw structure, the surgeon designs a plan that considers the patient’s preferences.
The procedure is generally carried out under local anesthesia. After the procedure is completed, the healing process begins. During this time, patients must follow their surgeon’s advice to ensure faster recovery and prevent potential complications.
How is Implant Surgery Performed in Men?
The implant surgery process for men is similar to that for women. The procedure for male patients is nearly identical for surgeons. However, there are a few differences. The jaw structure of men and women is distinct. Men's teeth are thicker and more square-shaped, while women's teeth are more rounded and have a thinner, more aesthetic appearance. Surgeons consider gender-specific features to ensure the prosthetic tooth appears more natural.
How is Implant Surgery Performed in Older Adults?
The process used for young and healthy individuals is also applicable to older patients, but special attention is given to factors such as bone density in elderly patients. Existing health issues and medications taken by elderly patients are carefully reviewed to design a safe procedure.
While the surgery is typically performed under local anesthesia, general anesthesia may be used depending on the patient’s health status. The surgeon carefully places the implant into the jawbone, usually completing this process quickly. Recovery time for older patients may be longer compared to younger patients due to age and health status. Once healing is complete, a permanent prosthetic tooth is placed.
How is Dental Implant Surgery Done?
Here is a step-by-step breakdown for those wondering, “How is dental implant surgery performed?”:
- Local anesthesia is administered to the patient. If a tooth extraction is required in the implant area, the tooth root is removed, and the area is cleaned and prepared for the implant.
- A small incision is made in the area where the implant will be placed, and the implant site is drilled with a specialized drill to accommodate the screw.
- The implant is covered with gum tissue and sutured.
- The screw inserted into the jawbone fuses with the bone within 2 to 6 months.
- A temporary prosthetic tooth can be placed based on the patient’s preference.
- Once complete integration with the jawbone is confirmed, the gum is reopened, and a connector piece is placed.
- An impression is taken of this connector piece to design a custom tooth for the patient.
- After the tooth is crafted, it is secured onto the implant with a connector piece known as an abutment.
Post-surgery, patients should attend regular check-ups and follow the surgeon’s instructions during the healing process.
What Are the Risks of Implant Surgery?
Implant surgery is generally considered safe with minimal risks. However, as with any surgical procedure, unexpected and unwanted outcomes may occur. There is a risk of infection, which is common in all surgeries, and surgeons may prescribe antibiotics to minimize this risk.
There is also a risk of damage to the jawbone during implant placement. An improperly placed or incorrectly sized implant may not integrate well with the jawbone, resulting in nerve damage, pain, swelling, and potential allergic reactions.
What Should I Do After Implant Surgery?
There are several post-operative guidelines to follow after implant surgery. Adhering to these rules helps ensure a smoother and healthier recovery after implant surgery.
Firstly, rest after the surgery and avoid heavy exercise for a while. Stick to soft foods for the recommended period, and avoid very hot or very cold drinks.
Pause any smoking and alcohol consumption. Keep your head elevated to reduce swelling. It’s also essential to maintain oral hygiene by brushing your teeth and keeping your mouth clean. However, avoid applying pressure to the implant area, and clean it with the mouthwash recommended by your doctor.
How Long Does It Take to Recover from Implant Surgery?
The recovery time after implant surgery varies depending on the procedure and the individual’s health status. Complete recovery may take several weeks or months due to the complex and multi-stage nature of the surgery.
The fusion process with the bone generally takes around 3 to 6 months, though patients can resume normal activities a few days after the initial procedure. A temporary prosthetic tooth can be placed until a permanent one is attached, extending the treatment and recovery period.
Frequently Asked Questions
How long does implant surgery take?
The duration varies depending on the number of implants, the patient’s health status, and potential complications during the procedure. However, in general, implant surgery takes about 1 to 3 hours to complete. For precise information, a detailed surgery plan should be prepared with the doctor.
How long do dental implants last?
The longevity of implants depends on material quality and how well the patient cares for them. With proper and regular care, dental implants can last for an extended period. With careful planning and attention to oral hygiene, they may even last a lifetime without any issues.
What are the advantages of dental implant surgery?
Your teeth appear very natural, with no sensation of having dentures, enhancing confidence. It is recommended for oral health, is highly durable, and can last for many years.
What is a Dental Bridge? How is it Made?
For optimal oral health, it is essential to have healthy teeth. However, in some cases, tooth loss may occur, leading to aesthetic concerns as well as functional issues in speaking and eating. A dental bridge is a method used to treat such cases of tooth loss.
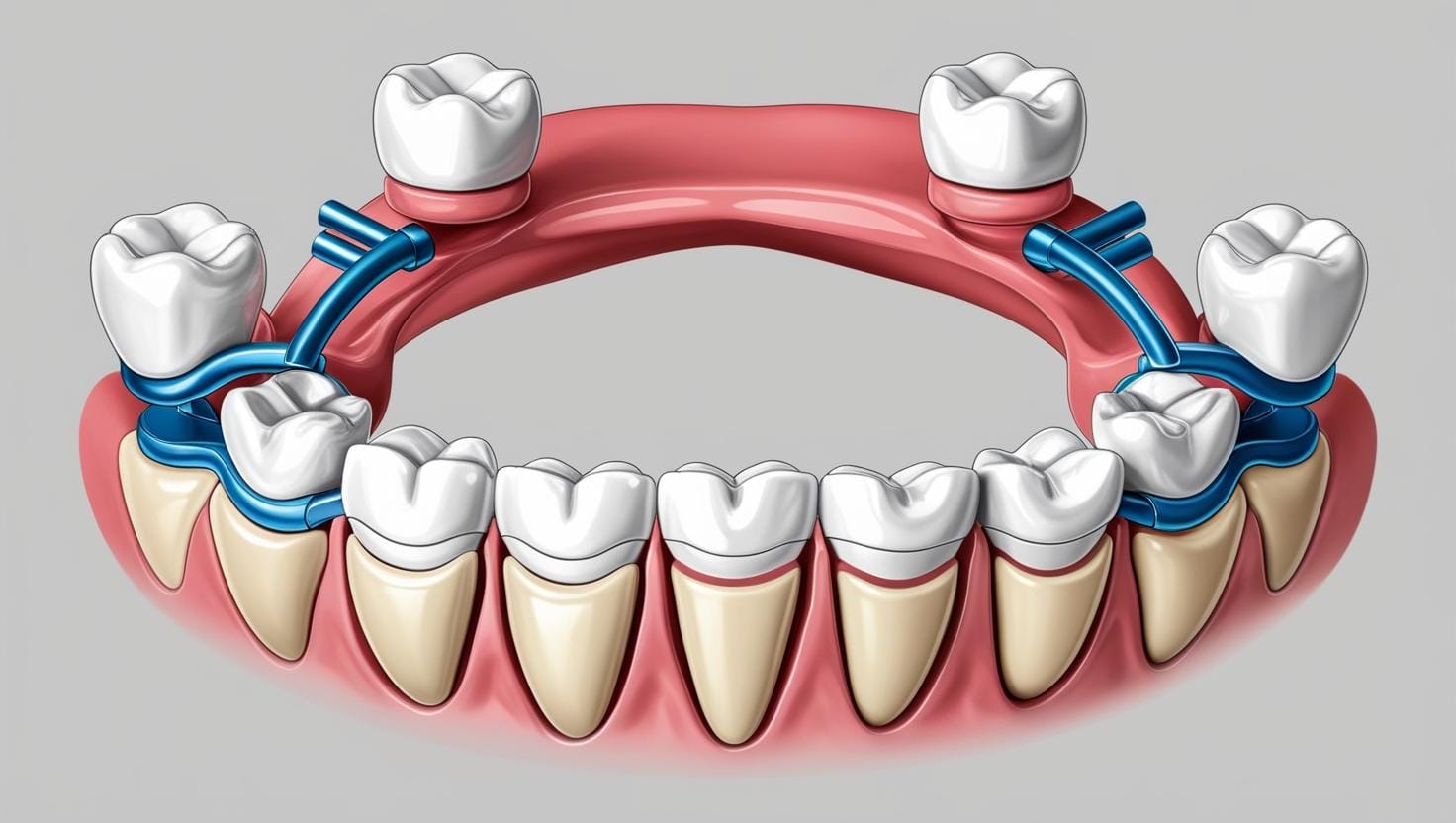
What is a Dental Bridge?
A dental bridge is a type of prosthesis used to replace one or several missing teeth, named for its design that resembles an actual bridge. The structure of a dental bridge consists of one or more artificial teeth that replace missing teeth. The sides of the bridge are prepared to rest on adjacent teeth using crowns that cover those neighboring teeth and secure the bridge in place.
Types of Dental Bridges
Dental bridges can be applied using various methods in oral treatment. Some of the most common types of dental bridges include:
- Traditional Bridges: These types of bridges are used to replace missing teeth and are supported by adjacent teeth. Traditional bridges are stable and durable.
- Cantilever Bridges: Used in cases where there is only one adjacent tooth supporting the bridge. This type of bridge is preferred if tooth loss occurs on only one side.
- Maryland Bridges: These bridges use metal clips or wings to attach to adjacent teeth, requiring less alteration to the tooth structure.
- Implant-Supported Bridges: These bridges rely on implant-supported teeth and are highly durable.

How is a Dental Bridge Made?
The application of a dental bridge involves a multi-step process performed by a dentist. The stages of dental bridge construction include:
- Examination and Preparation: First, the dentist designs and prepares the bridge to replace the missing teeth. The crowns or caps for the adjacent teeth are prepared.
- Taking Measurements: The prepared teeth are measured, and artificial teeth are created in a lab to fit the patient’s mouth structure.
- Temporary Bridge Fitting: While the artificial teeth are being made, the patient may need a temporary bridge. This temporary bridge can reduce aesthetic and functional problems during the waiting period.
- Permanent Bridge Placement: After the artificial teeth are produced and ready, the bridge is permanently placed in the mouth. The crowns covering the neighboring teeth secure the artificial teeth in place.
- Adjustments: Following the placement, the dentist makes necessary adjustments to the bridge to ensure proper biting and chewing functionality.
Advantages and Disadvantages of Dental Bridges
Dental bridges offer several advantages, although there may be a few disadvantages.
Advantages of Dental Bridges:
- Provide aesthetically pleasing results.
- Resolve missing teeth issues and restore chewing function.
- Can improve teeth alignment and spacing.
Disadvantages of Dental Bridges:
- The crowns or caps placed on neighboring teeth may require healthy teeth to be altered.
- The bridge may need replacement over time.
- Less durable than implants.
Who Can Get a Dental Bridge?
Oral health is an essential part of general health, and having healthy teeth positively affects daily life. However, sometimes teeth suffer from damage, loss, or aesthetic issues. Dental bridge treatment is a method used to address such problems by typically creating a bridge anchored to adjacent teeth to support a missing tooth. Recommended cases for dental bridge treatment include:
- Missing Teeth: Dental bridge treatment is used to replace missing teeth, which may result from trauma, decay, or other health issues. Dental bridges support the missing tooth and restore functionality.
- Oral Health: Good gum and tooth health is crucial for dental bridge treatment. Gum infections or severely decayed teeth should be addressed before treatment. A dental bridge should not be applied without treating these issues.
- Oral Hygiene: Maintaining oral hygiene is important after dental bridge treatment. The treated teeth and bridges should be brushed regularly, and dental floss should be used. Otherwise, decay and gum problems may reoccur.
- Healthy Adjacent Teeth: Dental bridge treatment requires strong neighboring teeth. The adjacent teeth support the bridge and bear the force applied during chewing. If there are significant problems with adjacent teeth, these issues may need to be resolved first.
Dental bridge treatment is an effective solution in cases recommended by a dentist. Since each patient's health condition is unique, treatment options vary from person to person.
What to Consider After Dental Bridge Treatment?
After dental bridge treatment, it may be necessary to take some protective measures to ensure the success of the treatment and the longevity of the treated teeth. These protective measures include:
- Regular Oral Hygiene: Following dental bridge treatment, maintaining regular oral hygiene by brushing teeth at least twice daily and using dental floss is essential. Dental bridges are prone to food debris and plaque accumulation, so attention should be given to oral cleanliness.
- Dental Checkups: Regular dental checkups may be required after dental bridge treatment. The dentist can monitor the condition of the bridge and gums and identify potential issues early on. It is generally recommended to have an oral examination twice a year.
- Avoiding Hard Foods: Although dental bridges are durable, excessively hard foods or objects can damage or dislodge the bridge. It may be necessary to avoid such items.
- Managing Teeth Grinding: If a person has a habit of grinding or clenching their teeth, it may be necessary to use a protective splint as recommended by the dentist. Teeth grinding can damage dental bridges.
- Balanced Nutrition: A healthy and balanced diet is important for maintaining general and oral health. Consuming enough calcium and other essential nutrients can strengthen teeth.
- Avoiding Smoking and Alcohol: Smoking and drinking alcohol can lead to gum disease and tooth loss. Such harmful habits should be avoided after dental bridge treatment.
- Protection from Trauma and Accidents: Protecting the mouth and teeth from trauma and accidents is essential for dental health following bridge treatment. Individuals engaging in high-risk sports or activities may need to use a mouthguard.
Taking protective measures after dental bridge treatment can enhance the success of the treatment and prolong the lifespan of the treated teeth. Patients must follow their dentist’s recommendations and instructions. Dental bridge treatment helps individuals regain oral health and achieve an aesthetically pleasing smile.
Frequently Asked Questions About Dental Bridges
Dental bridge treatment is a common choice to replace missing teeth, improve appearance, or restore oral health.
What Are the Costs of a Dental Bridge?
- The dentist examines the patient’s oral health to determine the condition of the teeth, the amount of bridge needed, the number of implants required, and the number of sessions involved. The cost of a dental bridge can vary depending on the treatment plan set by the dentist.
Is a Dental Bridge Procedure Painful?
- Dental bridge treatment is performed under local anesthesia to prevent sensitivity. The patient feels minimal discomfort beyond slight sensitivity.
Dental bridges offer an effective solution for replacing missing teeth. People who need dental bridge treatment should plan their treatment by scheduling an appointment with a dental clinic to restore a healthy oral structure.